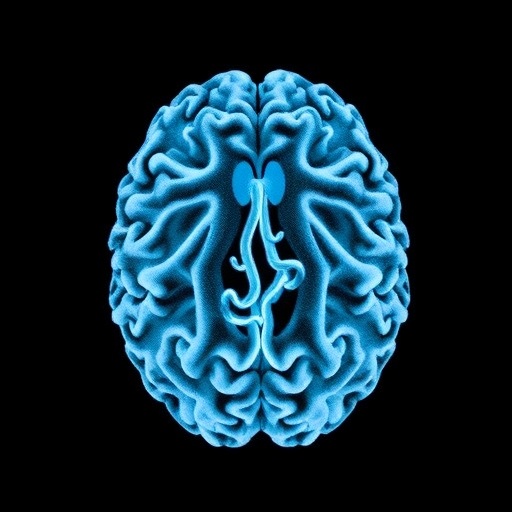
In a groundbreaking advancement in the neuroscience of suicidality, a new meta-analysis published in Translational Psychiatry unveils compelling evidence that structural brain abnormalities are intricately linked to suicidal thoughts and behaviors. This comprehensive study synthesizes data across numerous neuroimaging investigations, delivering unprecedented insight into the neural architecture that may underlie one of the most pressing public health crises worldwide. Far from merely mapping psychological distress, this research delves deep into the structural connectivity among critical brain regions, providing a biological substrate that could transform the future of suicide prevention and mental health diagnostics.
The research, led by Lim, Radua, and Beyh, represents the first large-scale meta-analytic effort to systematically quantify white matter disruptions associated with suicidality. Structural connectivity refers to the physical wiring of neural pathways, primarily formed by white matter tracts, which facilitate communication between disparate brain regions. Alterations in these pathways can impair cognitive, emotional, and regulatory functions, which are essential in maintaining psychological resilience. By consolidating data from multiple diffusion tensor imaging (DTI) studies, the authors illuminate consistent patterns of compromised connectivity, particularly in circuits implicated in emotional regulation, executive function, and impulse control.
To comprehend the neurobiological underpinnings of suicidal ideation and behaviors, this meta-analysis extracts common denominators from a heterogeneous body of literature. The technique of DTI is instrumental here, as it measures fractional anisotropy—a key indicator of white matter integrity—offering a quantitative lens into microstructural brain changes. By meticulously aggregating fractional anisotropy values from over a thousand subjects across diverse demographics and psychiatric diagnoses, the researchers gear towards resolving longstanding inconsistencies in neuroimaging findings related to suicidality.
One of the most striking revelations from this meta-analysis is the consistent disruption found in the anterior cingulum bundle, a white matter tract pivotal for cognitive control and emotional processing. The anterior cingulate cortex, connected via this bundle, has been extensively studied for its role in conflict monitoring and decision-making, functions that are often impaired in individuals exhibiting suicidal behavior. The decreased integrity in this pathway, the authors report, likely translates into the diminished capacity to regulate negative affect and inhibits adaptive responses to stress and pain, both psychological and physical.
Beyond the cingulum, the analysis highlights abnormalities in the uncinate fasciculus, a major white matter tract connecting the frontal lobe with the temporal lobe, including the amygdala. Given the amygdala’s central role in emotional salience and threat detection, disruptions in this tract could underlie heightened emotional reactivity and impaired top-down regulation—conditions frequently observed in suicidal individuals. This neurodevelopmental perspective suggests that aberrations in structural connectivity compromise the brain’s ability to modulate intense emotions, potentially making thoughts of suicide more salient and harder to suppress.
Another critical finding emerges in the corpus callosum, the largest commissural fiber bundle facilitating interhemispheric communication. The integrity of the corpus callosum ensures coordinated activity across both hemispheres, which is essential for integrating cognitive and affective information. Abnormalities in this structure, as revealed by the study, might contribute to fragmented cognitive processing and exacerbate dysregulated emotional states. This insight aligns with clinical observations of difficulty in problem-solving and emotional coherence in patients at risk of suicide.
The meta-analysis also underscores the complexity of suicidal behaviors by delineating structural differences between mere suicidal ideation and actual suicide attempts. The neural substrates demonstrating compromised integrity in attempters suggest a more severe disruption, especially in tracts tied to impulse control and reward processing. For instance, the frontostriatal pathways, which modulate goal-directed behavior and inhibitory control, show distinctly altered connectivity in those with a history of attempts compared to ideators, furnishing a biological basis for differentiating these crucial clinical phenotypes.
Methodologically, the authors employed rigorous inclusion criteria and advanced statistical approaches to mitigate bias and enhance the reliability of findings. The use of coordinate-based meta-analysis allowed for the integration of spatial brain data, while addressing heterogeneity across studies and scanner modalities. This robust framework not only affirms previously hypothesized connectivity disruptions but also opens avenues for identifying novel neuroanatomical targets that have eluded smaller individual studies.
Importantly, the paper situates these structural findings within a broader neurobiological and psychological framework, emphasizing that connectivity disruptions do not operate in isolation but interact dynamically with environmental and genetic risk factors. This neurocircuitry lens integrates how early-life stress, trauma, and chronic psychiatric conditions may converge with structural vulnerabilities, precipitating suicidal crisis. Such a multidimensional model enhances the clinical relevance, suggesting that interventions need to be tailored to these neurobiological profiles to optimize prevention strategies.
The authors advocate for the incorporation of these neuroimaging biomarkers into clinical practice, envisioning a future where an individual’s structural connectivity profile informs personalized risk assessment. This anticipatory approach could revolutionize current protocols which primarily rely on subjective reports and psycho-social factors. Early identification of at-risk individuals through brain imaging could enable timely, targeted interventions, potentially averting fatal outcomes.
Moreover, this extensive analysis also raises pertinent questions about neuroplasticity and treatment implications. Can disrupted connectivity be restored through pharmacological agents, cognitive therapies, or neuromodulation techniques such as transcranial magnetic stimulation? The correlation between white matter integrity and suicidal risk encourages further research into therapies that promote white matter repair or functional compensation as novel suicide prevention strategies.
The study, while comprehensive, acknowledges limitations related to the cross-sectional nature of most included studies, the variability of diagnostic categories, and the technical heterogeneities inherent in neuroimaging data acquisition. Longitudinal studies are necessary to disentangle whether observed connectivity changes are a cause or consequence of suicidality. Additionally, larger, more diverse cohorts would enhance the generalizability of these neurobiological signatures across populations.
Ethical considerations also come to the forefront, as the translation of brain-based risk profiling into practice must be handled with sensitivity to avoid stigmatization or determinism. The potential misuse of neuroimaging data demands robust safeguards to ensure that findings empower rather than marginalize vulnerable individuals.
Taken together, this meta-analysis marks a transformative milestone in suicide research. By elucidating the structural connectivity disturbances underlying suicidality, it transcends traditional symptom-based paradigms and accelerates a neurobiologically informed understanding of suicide risk. As the field moves forward, these insights could catalyze the development of highly specific diagnostic tools and personalized interventions, ultimately reducing the tragic global burden of suicide.
In the rapidly evolving landscape of psychiatric neuroscience, this work exemplifies the power of large-scale integrative analyses to decode complex brain-behavior relationships. The fusion of cutting-edge neuroimaging and meta-analytic rigor not only enhances scientific clarity but also offers hope for novel, effective strategies against a condition that has long confounded clinicians and researchers alike.
Future investigations building on this foundation will hopefully refine these neurobiological markers further, delineate causal pathways, and explore mechanistic interventions that restore structural connectivity. Such advances could shift the paradigm from reactive crisis management to proactive, preemptive mental health care informed by the brain’s intricate wiring patterns.
Ultimately, the promise of this research lies in its potential to save lives. By shining a spotlight on the hidden architecture of suicidal vulnerability, it underscores the urgency and feasibility of developing brain-based solutions in the global endeavor to combat suicide.
Subject of Research: Structural connectivity abnormalities in suicidal thoughts and behaviours
Article Title: Structural connectivity abnormalities in suicidal thoughts and behaviours: a meta-analysis
Article References:
Lim, L., Radua, J. & Beyh, A. Structural connectivity abnormalities in suicidal thoughts and behaviours: a meta-analysis. Transl Psychiatry 15, 480 (2025). https://doi.org/10.1038/s41398-025-03699-4
Image Credits: AI Generated
DOI: 10.1038/s41398-025-03699-4