In a groundbreaking study published in Nature Communications, researchers have unveiled a critical neurological fingerprint characterizing status dystonicus, an often overlooked and severe manifestation of dystonia. This research pioneers our understanding of the electrophysiological underpinnings of this acute dystonic crisis, specifically highlighting a unique beta-band activity pattern within the globus pallidus, a deep brain structure pivotal to motor control.
Dystonia, a neurological movement disorder typified by involuntary muscle contractions resulting in repetitive or twisting movements, can escalate into a life-threatening emergency known as status dystonicus (SD). Despite its clinical severity, the exact neurophysiological basis of SD has remained shrouded in mystery, limiting targeted therapeutic options. The study by Balachandar et al. provides compelling evidence that SD represents a distinct neurophysiological state, demarcated by a pronounced elevation in pallidal beta-band oscillations, which may serve as both a biomarker and a therapeutic target.
The authors conducted an extensive electrophysiological investigation on patients experiencing SD, utilizing intracranial recordings to detect oscillatory activity within basal ganglia circuits. Their data demonstrate that beta-band activity (13–30 Hz), typically associated with motor control and pathological synchronization in other movement disorders like Parkinson’s disease, is significantly augmented during SD episodes. This finding challenges the traditional classification of dystonia solely as a hypo-synchronous disorder and suggests a more nuanced pathophysiological spectrum involving abnormal hyper-synchronization in pallidal networks.
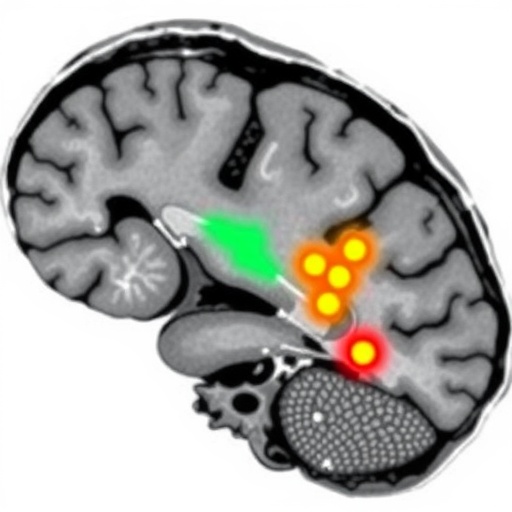
Intriguingly, the exacerbated beta-band activity observed localized predominantly to the internal segment of the globus pallidus (GPi). This structure, integral to the indirect pathway of the basal ganglia, modulates inhibitory output to motor thalamus and cortex, thereby regulating movement. The heightened beta oscillations may reflect dysfunctional inhibitory signaling within these motor circuits, precipitating the uncontrollable muscle contractions characteristic of SD. By pinpointing this electrophysiological signature, the study lays groundwork for refining neuromodulatory interventions that target these aberrant beta rhythms.
The implications of this discovery are manifold. From a clinical perspective, the ability to identify a distinct beta-band oscillation pattern during SD could enhance diagnostic precision, facilitating earlier recognition and tailored management of dystonic crises. Further, it offers a mechanistic rationale for the observed efficacy of deep brain stimulation (DBS) targeting the GPi, which is thought to disrupt pathological beta synchronization. Fine-tuning DBS parameters to specifically counteract beta-band activity might improve outcomes in patients resistant to pharmacological therapies.
Moreover, this beta-band hyperactivity might serve as a biomarker for monitoring disease progression and treatment response in dystonia more broadly. The study’s findings suggest that beta oscillations could be leveraged for closed-loop neuromodulation systems, where real-time detection of pathological rhythms triggers adaptive stimulation, optimizing therapeutic efficacy while minimizing side effects. Such biofeedback-driven treatments represent the frontier of personalized neurology.
Notably, the research incorporated a multi-modal approach integrating neurophysiology, clinical observation, and computational analyses to validate the distinctness of SD’s neural signature. This holistic methodology underscores the complexity of movement disorders and the necessity of converging techniques to decode their mechanistic intricacies. Furthermore, it exemplifies how electrophysiological signatures can transform our conceptual frameworks, reframing disorders like SD from vague clinical syndromes to well-defined neurodynamic entities.
The elevated beta-band activity contrasts with the oscillatory profiles reported in other dystonic states, where abnormal theta or gamma rhythms have been implicated. This divergence not only emphasizes SD’s uniqueness but also prompts re-examination of basal ganglia circuitry across dystonia subtypes. A refined taxonomy based on electrophysiological phenotypes could yield nuanced therapeutic stratification, enabling clinicians to harness distinct neural targets for different dystonia variants.
Importantly, the study contributes to the evolving narrative that motor disorders are underpinned by maladaptive neural oscillations disrupting circuit homeostasis. The basal ganglia’s centrality in this pathological rhythmicity highlights its dual role as a generator and modulator of motor patterns. Unraveling these oscillatory dynamics opens vistas for novel pharmacological strategies aimed at restoring synaptic and network balance, complementing existing interventional techniques like DBS and botulinum toxin injections.
From a technological standpoint, the study showcases advanced electrophysiological recording capabilities facilitated by implantable devices, enabling high-fidelity monitoring of deep brain activity in real time. These innovations are critical for translating bench discoveries into bedside applications, allowing clinicians to tailor interventions based on objective neural markers. Such progress heralds an era where bioelectronic medicine could transform treatment paradigms across neuropsychiatric and movement disorders.
The authors also emphasize that their findings necessitate further longitudinal studies to ascertain how pallidal beta-band oscillations evolve during the natural history of dystonia and its acute exacerbations. Understanding temporal dynamics could illuminate triggers and early warning signs of SD, opening avenues for preemptive therapeutic interventions. Moreover, characterizing inter-individual variability in beta oscillations may inform personalized risk profiling and intervention strategies.
In closing, this seminal research marks a paradigm shift in the understanding of status dystonicus, establishing its neurophysiological distinctiveness through the lens of pallidal beta oscillations. By bridging clinical phenomenology with cutting-edge neurophysiology, it paves the way toward precision neuromodulation therapies and improved patient outcomes. As technologies evolve and interdisciplinary collaborations deepen, the hope for effective management of dystonic crises becomes ever more attainable.
The elucidation of beta-band activity as a hallmark of status dystonicus not only deepens the scientific community’s grasp of basal ganglia pathophysiology but also galvanizes future research aimed at translating these insights into tangible clinical interventions. This discovery underscores the profound potential of neural oscillations as both diagnostic biomarkers and therapeutic targets, reinforcing the burgeoning field of oscillopathy-focused neuroscience.
Future research inspired by this study will likely explore the modulation of beta rhythms through pharmacological, genetic, and behavioral therapies, striving to recalibrate dysfunctional motor networks implicated in dystonia. The integration of electrophysiological biomarkers with genomic and proteomic data could usher in a new era of multifaceted, individualized care paradigms for patients battling this disabling disorder.
In essence, the work of Balachandar and colleagues establishes a foundational cornerstone in dystonia research, illuminating the enigmatic status dystonicus through the prism of pallidal beta-band activity. Their insights offer a beacon of hope for patients and clinicians alike, heralding an age where acute dystonic crises can be precisely defined, predictably managed, and ultimately, prevented.
Subject of Research: Neurophysiological characterization of status dystonicus via pallidal beta-band oscillations
Article Title: Status dystonicus is a distinct state characterized by pallidal beta-band activity
Article References:
Balachandar, A., Vogt, L.M., Mithani, K. et al. Status dystonicus is a distinct state characterized by pallidal beta-band activity. Nat Commun 16, 9352 (2025). https://doi.org/10.1038/s41467-025-64416-9
Image Credits: AI Generated