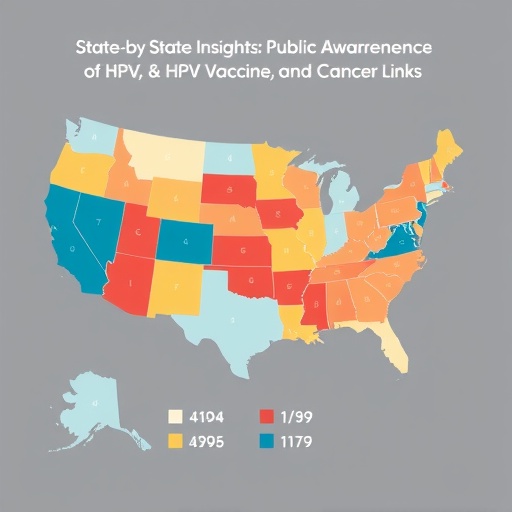
In a revealing new cross-sectional study published in JAMA Oncology, researchers have uncovered strikingly low levels of public awareness regarding human papillomavirus (HPV), the HPV vaccine, and the well-established relationship between HPV infection and numerous types of cancers. This lack of knowledge appears especially acute in the Midwestern and Southern regions of the United States—geographic areas where HPV-associated cancers are surging at alarming rates. The findings shed light on a critical public health gap that may significantly hinder prevention efforts, particularly in locales that have historically lagged behind in vaccination uptake.
HPV is a ubiquitous virus with more than 200 known types, some of which are directly implicated in the pathogenesis of cervical, oropharyngeal, anal, and other anogenital cancers. Despite this, the general population’s understanding of HPV’s oncogenic potential remains insufficient. The study’s data suggest that even as HPV-related cancer incidence climbs, public knowledge about the virus and the availability and efficacy of vaccination to prevent these cancers is alarmingly limited. In epidemiological terms, this disconnect is particularly troubling because it perpetuates vulnerability within populations already experiencing higher disease burdens.
A deeper dive into the study reveals a strong correlation between geographic regions marked by low HPV awareness and those with suboptimal vaccination coverage. Many Midwestern and Southern states show HPV vaccination rates well below the national average, compounding their risk profile. This relationship highlights the multifaceted challenges underpinning public health messaging and vaccine advocacy in these areas, possibly influenced by socioeconomic, cultural, and political factors that impede effective outreach and education.
The HPV vaccine represents a major breakthrough in preventive oncology, with prophylactic vaccines proven to substantially reduce infection rates of the high-risk HPV strains responsible for the majority of HPV-attributable cancers. However, awareness and acceptance of HPV vaccination remain uneven across the United States. Vaccination coverage disparities reflect underlying disparities in healthcare access, insurance status, and educational outreach, factors that are spatially patterned and coalesce in these vulnerable U.S. regions.
From a virological standpoint, HPV infects epithelial tissues and can integrate its DNA into host cells, causing genomic instability that drives malignant transformation. The virus’s oncogenic mechanisms often involve the viral oncoproteins E6 and E7, which interfere with tumor suppressor proteins p53 and Rb. Understanding these molecular interactions underscores the critical need for effective prevention, as once HPV-induced carcinogenesis begins, therapeutic options become significantly more complicated and resource-intensive.
The study’s findings provide a stark reminder that the battle against HPV-associated cancers cannot depend solely on the existence of a vaccine; comprehensive public education and targeted healthcare policies are indispensable. The researchers emphasize that public health strategies must evolve to address awareness deficits, particularly in the Midwestern and Southern states, through culturally sensitive communication methodologies that resonate with local populations and dismantle barriers rooted in misinformation or distrust.
In the realm of public health policy, the implications are profound. With HPV-associated cancers contributing significantly to cancer morbidity and mortality, especially among underserved populations, it is imperative to align vaccination campaigns with community engagement initiatives. These must be tailored to address the sociocultural contexts of the Midwest and South, incorporating the input of local healthcare providers, educators, and community leaders to amplify message penetration and vaccine acceptance rates.
The study further interrogates regional demographic variables that may influence HPV awareness and vaccine uptake, including but not limited to education level, income brackets, urban versus rural status, and healthcare provider density. Patterns emerging from this data suggest that public health interventions must be multifactorial and precise, leveraging epidemiologic surveillance data to deploy resources where they are most needed and likely to be effective.
This investigation also highlights a critical temporal aspect: as the incidence of HPV-linked cancers rises, the urgency to increase vaccination rates and public understanding becomes ever more acute. Delays or failures in addressing these gaps risk further entrenching cancer disparities and exacerbating the burden on healthcare systems. Moreover, understanding public perceptions, myths, and hesitancies surrounding the HPV vaccine will be pivotal in designing interventions that not only inform but also transform behaviors.
The research underscores the role of healthcare providers as key messengers in HPV education and vaccine promotion. Provider recommendation has been identified in numerous studies as one of the strongest predictors of vaccine uptake. Hence, empowering clinicians with updated training and communication tools to discuss HPV-related risks and preventive options is a lynchpin in reversing current trends of low awareness and vaccination.
Additionally, technological advances in vaccine formulation and delivery, including the advent of nonavalent HPV vaccines covering nine HPV strains and novel administration schedules, present new opportunities to enhance preventive efficacy. Public awareness must keep pace with these scientific developments to maximize public health benefits. Integrating these technical advancements into educational content will empower the public to make informed decisions grounded in the latest evidence.
In conclusion, this compelling study serves as an urgent call to action for policymakers, healthcare professionals, and community stakeholders. The nexus of low HPV awareness, mounting HPV-associated cancer incidence, and suboptimal vaccination coverage, particularly in the Midwest and South of the United States, represents a significant public health challenge. To stem the tide of preventable cancers, a concerted, science-driven, and culturally tailored approach is essential—one that elevates awareness, fortifies vaccine advocacy, and bridges the knowledge gap that currently hinders effective cancer prevention.
Subject of Research: Public awareness and vaccination rates related to human papillomavirus (HPV) and HPV-associated cancers in regions of the United States.
Article Title: [Not provided]
News Publication Date: [Not provided]
Web References: [Not provided]
References: (doi:10.1001/jamaoncol.2025.2638)
Image Credits: [Not provided]
Keywords: Cancer; Vaccine research; Vaccination; Viruses; Public health; United States population; Geographic regions; Oncology