In a groundbreaking study published in Cell Death Discovery, researchers have made a significant leap in understanding the molecular mechanisms underlying ovarian cancer, a malignancy notorious for its poor prognosis and resistance to conventional therapies. The investigation led by Nie, R., Zhou, H., Chen, L., and colleagues reveals that targeting the transcription factor SREBP1 sensitizes ovarian cancer cells to ferroptosis, a form of programmed cell death distinct from apoptosis, by impairing the Nrf2-XCT/GPX4 antioxidant axis. This insight not only opens new therapeutic avenues but also bridges critical gaps in the intricate network of cancer metabolism and cell death regulation.
Ovarian cancer remains one of the deadliest gynecological cancers globally, often diagnosed at advanced stages due to subtle early symptoms. Despite advances in chemotherapy and targeted therapies, relapse and resistance remain significant challenges, driving the urgency to identify novel vulnerabilities within cancer cells. Ferroptosis, characterized by iron-dependent lipid peroxidation, has emerged as a promising cell death modality that could be exploited therapeutically. However, the molecular regulators orchestrating ferroptosis in ovarian cancer have not been fully elucidated.
In this landmark research, SREBP1 (sterol regulatory element-binding protein 1), a key transcription factor primarily known for regulating lipid biosynthesis, was found to play an unexpected but crucial role in ferroptosis resistance. The authors demonstrated that knocking down SREBP1 in ovarian cancer cell lines triggered extensive ferroptotic cell death. This discovery challenges previous paradigms that mainly associated SREBP1 with metabolic functions, placing it at the epicenter of cancer cell survival and death pathways.
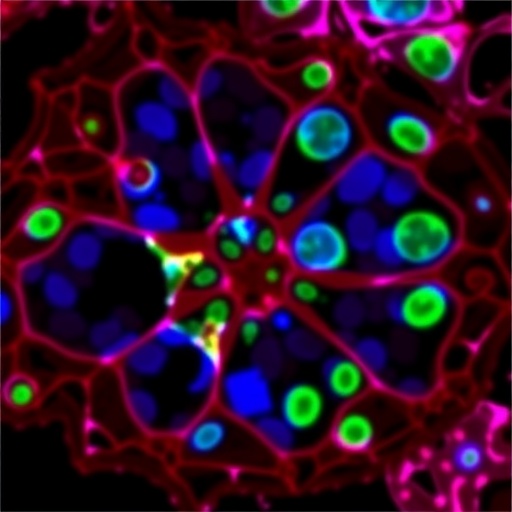
Detailed mechanistic analyses revealed that suppressing SREBP1 led to the downregulation of the Nrf2-XCT/GPX4 axis, a vital antioxidant defense system that protects cells from oxidative damage. Nrf2 (nuclear factor erythroid 2-related factor 2) is a master regulator of cellular redox homeostasis, driving the expression of genes like XCT (SLC7A11, a cystine/glutamate antiporter) and GPX4 (glutathione peroxidase 4), both essential for neutralizing lethal lipid peroxides. The disruption of this axis by SREBP1 knockdown impaired the cancer cells’ ability to detoxify reactive oxygen species, culminating in ferroptosis.
The study utilized a comprehensive approach, integrating gene knockdown techniques, lipid peroxidation assays, and ferroptosis markers assessment, to establish a causal relationship between SREBP1 activity and ferroptosis resistance. The data showed that reducing SREBP1 expression lowered XCT and GPX4 levels, thereby weakening the antioxidant defenses. Notably, this vulnerability was not a generic oxidative stress response but specific to the ferroptotic pathway, highlighting a targeted mechanistic link.
Importantly, the research indicates that SREBP1 acts upstream of Nrf2, suggesting a regulatory hierarchy where lipid metabolism and antioxidant responses converge. This connection is particularly compelling given cancer cells’ reliance on altered lipid metabolism for growth and survival. By controlling the Nrf2-XCT/GPX4 axis, SREBP1 integrates metabolic and redox signals to enhance cancer cell resilience against ferroptotic stress.
The implications of these findings are profound for therapeutic development. Inhibiting SREBP1 or disrupting its downstream antioxidant machinery could sensitize ovarian cancer cells to ferroptosis-inducing agents, potentially overcoming drug resistance. This strategy might complement existing treatments, providing a two-pronged attack on cancer cells by simultaneously targeting metabolism and cell death pathways.
Moreover, the study sheds light on the metabolic plasticity of ovarian cancer. The ability to manipulate the redox environment through the SREBP1-Nrf2-XCT/GPX4 axis reflects the cancer’s adaptability to oxidative stress. Therapeutic interventions designed to dismantle this axis could tip the balance towards cell death, making ferroptosis a more accessible endpoint for cancer elimination.
This research also underscores the need to further explore SREBP1’s broader interactions within the tumor microenvironment. Given the pivotal role of antioxidants in immune evasion and therapy resistance, understanding how SREBP1 influences these processes could unveil additional targets for combinatorial treatments, enhancing the efficacy of immunotherapies.
In the context of personalized medicine, assessing SREBP1 expression levels in ovarian cancer patients might serve as a biomarker to predict responsiveness to ferroptosis-based therapies. Patients exhibiting high SREBP1 activity could potentially benefit from SREBP1 inhibitors or agents that disrupt the Nrf2-XCT/GPX4 axis, aligning treatment choices with molecular tumor profiles.
The study also raises intriguing questions about the universality of SREBP1’s role across other cancer types. Given the ubiquitous nature of lipid metabolism and redox regulation in various malignancies, similar ferroptosis-related vulnerabilities may exist, warranting broader investigations. Such cross-cancer studies could lead to the development of pan-cancer ferroptosis sensitizers targeting SREBP1 or its downstream effectors.
Furthermore, the downstream molecular consequences of SREBP1 inhibition on cellular metabolism and survival pathways merit deeper analysis. For instance, how do alterations in lipid composition influence membrane susceptibility to peroxidation? Do SREBP1-regulated lipids play structural or signaling roles that modulate ferroptotic signaling cascades? Unpacking these layers will enrich our understanding of lipid biology in cancer.
As with many pioneering discoveries, translation to clinical practice faces challenges, including the specificity and safety of potential SREBP1 inhibitors. Developing agents that selectively target cancer cells without disrupting normal lipid homeostasis is crucial. In this regard, the tumor-specific dependencies on the SREBP1-Nrf2-XCT/GPX4 axis might offer a therapeutic window to minimize toxicity.
The study by Nie et al. thus not only advances the fundamental understanding of ovarian cancer biology but also charts a promising course towards novel, mechanism-based therapies. By revealing the intersection of lipid metabolism and ferroptosis regulation via SREBP1, the research highlights an exploitable vulnerability that could revolutionize treatment paradigms.
In summary, the identification of SREBP1 as a master regulator that safeguards ovarian cancer cells from ferroptosis by modulating the Nrf2-XCT/GPX4 antioxidant axis presents a paradigm-shifting perspective. This discovery enriches the landscape of cancer metabolism, oxidative stress, and programmed cell death, offering hope for the development of innovative therapies that could improve outcomes for ovarian cancer patients worldwide.
Subject of Research: The role of SREBP1 in regulating ferroptosis through the Nrf2-XCT/GPX4 antioxidant axis in ovarian cancer.
Article Title: SREBP1 knockdown triggers ferroptosis by suppressing the Nrf2-XCT/GPX4 axis in ovarian cancer.
Article References:
Nie, R., Zhou, H., Chen, L. et al. SREBP1 knockdown triggers ferroptosis by suppressing the Nrf2-XCT/GPX4 axis in ovarian cancer. Cell Death Discov. (2026). https://doi.org/10.1038/s41420-026-02964-9
Image Credits: AI Generated