In recent years, the role of smooth muscle cells (SMCs) in arterial health and disease has garnered significant attention. Understanding the molecular mechanisms by which these cells contribute to vascular conditions, particularly intimal hyperplasia following arterial injury, is critical in developing effective therapeutic strategies. A compelling study published in the Journal of Biomedical Science explores this phenomenon, shedding light on the impact of hydroxyindole O-methyltransferase (HIOMT) expression specifically within smooth muscle cells.
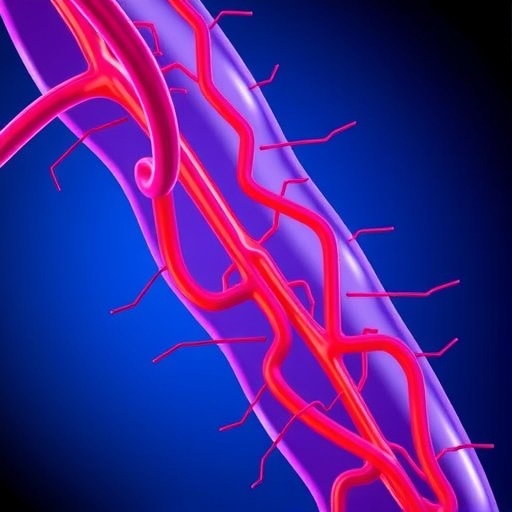
The study highlights a transformative discovery: the expression of HIOMT in smooth muscle can markedly reduce arterial injury-induced intimal hyperplasia. This pathophysiological condition arises when there is injury to the arterial wall, leading to an excessive proliferation of smooth muscle cells, contributing to the thickening of the vessel wall and narrowing of the lumen. Such events can predispose individuals to severe cardiovascular complications, including ischemia and thrombosis.
The research team, led by Jiang et al., performed a series of meticulous experiments to elucidate the cellular and molecular consequences of HIOMT expression in SMCs. By utilizing advanced genetic modification techniques, the researchers engineered mice to selectively express HIOMT in smooth muscle cells. This well-thought-out approach provided a focused lens through which the effects of HIOMT could be observed in isolation from other cell types.
One of the hallmark features of intimal hyperplasia is the transition of smooth muscle cells from a contractile phenotype to a proliferative one. This process is underpinned by complex signaling pathways that are modulated by various growth factors and cytokines. The findings from Jiang and colleagues indicate that enhanced HIOMT expression interferes with these pathways, specifically by altering the response of SMCs to proliferative signals. As such, this manipulation prevents the excessive cell growth that typifies intimal hyperplasia.
HIOMT is an enzyme critical for the metabolism of serotonin and other indoleamine substances. By influencing serotonin levels, the expression of HIOMT in vascular smooth muscle cells appears to have a cascading effect on SMC behavior. Serotonin is known for its role not only in neurotransmission but also in various vascular processes, including vasoconstriction and modulation of vascular smooth muscle proliferation. Consequently, increasing HIOMT activity may lead to reduced levels of bioactive serotonin in the vicinity of the arterial wall, blunting the pathological cellular responses associated with arterial injury.
What makes the work of Jiang et al. particularly exciting is the translational potential of their findings. The ability to modulate smooth muscle cell function through pharmacological or genetic means opens new avenues for intervention in cardiovascular diseases marked by intimal hyperplasia. For instance, targeted therapies that enhance HIOMT function or mimic its effects could become a cornerstone in the prevention of complications arising from arterial injury.
Furthermore, the study reinforces the importance of understanding the local cellular environment in the development of therapeutic strategies. Many existing treatments have focused on systemic approaches, but the specificity of HIOMT’s effects suggests that localized interventions may yield more effective outcomes with fewer side effects. Targeted delivery systems that can amplify HIOMT activity specifically in SMCs could revolutionize how we address vascular pathologies.
In response to the tantalizing implications of this research, the scientific community is likely to see a surge of interest in HIOMT and its regulatory mechanisms within smooth muscle cells. Subsequent studies will undoubtedly seek to explore the wider biological implications of these findings, particularly in human models. This will involve dissecting the precise pathways through which HIOMT exerts its effects and establishing whether similar outcomes can be replicated in human vascular tissue.
However, as with any promising avenue of research, challenges remain. Future studies must explore the safety and efficacy of manipulating HIOMT levels in a clinical context. The long-term implications of altering smooth muscle cell behavior must be thoroughly assessed to ensure that potential therapies do not inadvertently lead to adverse outcomes. The balance between preventing intimal hyperplasia and maintaining normal vascular function is delicate, necessitating a nuanced approach in future research and therapeutic development.
In summary, Jiang et al.’s research illuminates a novel molecular mechanism governing smooth muscle cell behavior in the context of arterial injury. By demonstrating that enhanced expression of HIOMT can inhibit intimal hyperplasia, the study not only provides insight into the complex dynamics of vascular biology but also holds promise for innovative therapeutic strategies. As the scientific community delves deeper into the implications of this work, the hope is to foster breakthroughs that will ultimately lead to improved cardiovascular health outcomes.
The implications of this research extend beyond mere academic intrigue; they have the potential to reshape treatment paradigms for patients with a predisposition to vascular disease. As we stand on the cusp of new discoveries in cardiovascular therapeutics, the work of Jiang and colleagues serves as a beacon of hope, emphasizing the importance of targeted biological research in unearthing solutions to prevalent health challenges.
Furthermore, the broader context in which this research exists cannot be overlooked. With the increasing prevalence of lifestyle-related vascular conditions, this study is timely and reinforces the critical need for ongoing research in vascular biology. As scientists continue to explore the intricate interplay between genetic, environmental, and lifestyle factors, the potential for breakthroughs that could significantly alter patient outcomes remains palpable.
In conclusion, the research conducted by Jiang and his team is a testament to the ingenuity and dedication of modern science. It reflects a concerted effort to understand complex biological systems and translate that knowledge into actionable therapeutic strategies. As we continue to explore the molecular intricacies of vascular health, we must embrace the challenges and opportunities that lie ahead, aiming ultimately to improve patient care and enhance quality of life through innovative medical solutions.
Subject of Research: Hydroxyindole O-methyltransferase in Smooth Muscle Cells and its Effect on Intimal Hyperplasia
Article Title: Smooth muscle-specific expression of hydroxyindole O-methyltransferase reduces arterial injury-induced intimal hyperplasia.
Article References:
Jiang, WC., Chen, CH., Ho, HH. et al. Smooth muscle-specific expression of hydroxyindole O-methyltransferase reduces arterial injury-induced intimal hyperplasia.
J Biomed Sci 32, 78 (2025). https://doi.org/10.1186/s12929-025-01172-4
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12929-025-01172-4
Keywords: smooth muscle cells, hydroxyindole O-methyltransferase, intimal hyperplasia, arterial injury, cardiovascular health, therapeutic strategies