Neuroscience has often been at the forefront of cutting-edge research, particularly in understanding the complexities of neurodegenerative diseases. A recent study published in BMC Neuroscience has shed light on the intricate relationship between inflammation and neuronal health, specifically examining the effects of lipopolysaccharide (LPS) treatment on astrocytes in the context of Parkinson’s Disease. The research primarily focuses on LRRK2 G2019S knock-in mice, a model that provides invaluable insights into the underlying mechanisms of this debilitating condition.
The use of LPS, a component of the outer membrane of gram-negative bacteria, has conventionally been associated with the induction of systemic inflammation. Its application in laboratory settings to study neuroinflammation reveals the intricate network of cellular interactions that occur in response to inflammatory stimuli. In the current study, researchers administered short-term LPS treatment to LRRK2 G2019S knock-in mice, aiming to explore how astrocytes—glial cells that play a pivotal role in maintaining the homeostasis of the central nervous system—respond to such challenges.
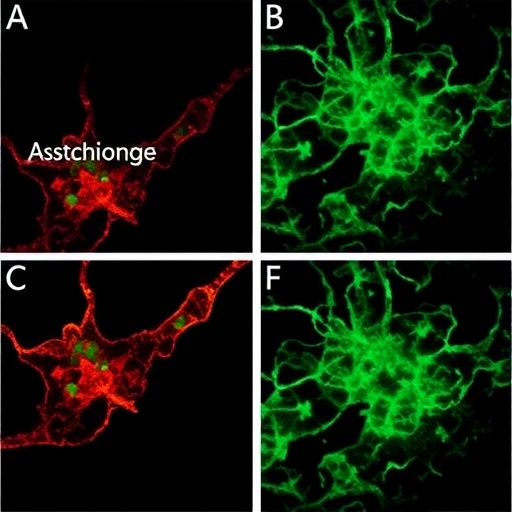
Astrocytes are not merely passive supporters of neuronal function; they actively participate in synaptic maintenance and neurotransmitter recycling among other essential tasks. In the context of Parkinson’s Disease, where dopaminergic neurons are selectively vulnerable, assessing the activation state of astrocytes could provide crucial insights into compensatory mechanisms that may protect against neuronal death. In the LRRK2 G2019S model, researchers observed significant astrocyte activation following LPS treatment, signaling a robust inflammatory response that merits further investigation.
While many studies have previously linked chronic inflammation with neuronal cell death, the findings of this research are particularly intriguing because they highlight that short-term inflammatory episodes do not necessarily culminate in immediate neuronal loss. In fact, researchers reported no evident loss of dopaminergic neurons following the LPS exposure. This finding posits a hopeful perspective that short-lived inflammatory signals might invoke a protective astrocytic response rather than leading to neurodegeneration. The implications are profound, suggesting that timely inflammatory events may activate neuroprotective pathways rather than detract from neuronal survival.
The specific pathways activated in astrocytes in response to LPS represent a fascinating area of inquiry. Hormonal signals through receptors on the astrocyte membranes may mediate either pro-inflammatory or anti-inflammatory pathways depending on the duration and intensity of the inflammatory cues. Researchers utilized immunohistochemical staining techniques to analyze the expression of glial fibrillary acidic protein (GFAP), a marker indicative of astrocytic activation. The elevated GFAP levels post-LPS treatment confirm that astrocytes assumed an activated state, possibly indicative of their role in neuroprotection.
Interestingly, the study also delves into the signaling cascades implicated in astrocyte activation. The activation of pathways, such as the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-kB) signaling pathway, plays a crucial role in regulating the inflammatory response within the brain. By dissecting these pathways, scientists can better understand how astrocytes transition from a protective to a potentially harmful role. Knowledge of these transitions could guide therapeutic strategies aimed at enhancing astrocyte function in a way that would benefit neuroprotection while minimizing neuroinflammation.
The specificity of the LRRK2 G2019S model also lends itself to discussions about genetic predispositions and their implications for neuroinflammatory responses. Mutations in the LRRK2 gene have been linked to familial forms of Parkinson’s Disease, and studying these knock-in mice allows researchers to explore the intersection between genetic factors and environmental triggers such as inflammation. Through this lens, the roles of genetic modifiers in disease progression become clearer, igniting discussions on personalized approaches in treating inflammatory-related neurodegenerative diseases.
As the scientific community continues to unfold the complexities of the brain’s immune response, findings from this research reaffirm the necessity for longitudinal studies to assess long-term outcomes following short-term inflammatory events. It would be enlightening to determine whether astrocytes maintain their protective phenotype over extended periods post-inflammation or if prolonged challenges lead to their eventual dysfunction—a transition that is often seen in chronic inflammatory states.
Moreover, understanding the interplay between astrocyte activation and dopaminergic neuron resilience has implications beyond Parkinson’s Disease. The findings prompt further exploration into several neurodegenerative diseases where neuroinflammation is a significant hallmark. Could similar astrocytic activation be observed in Alzheimer’s Disease or Amyotrophic Lateral Sclerosis (ALS)? These questions highlight the study’s broader relevance to the field of neurodegeneration and neuroinflammation.
The research’s outcomes necessitate a paradigm shift in how we perceive inflammation in the central nervous system. Instead of viewing inflammation solely as a destructive process, it is essential to appreciate its dual nature—both beneficial and detrimental—especially in the context of neurodegenerative diseases. This nuanced understanding can revolutionize therapeutic approaches, focusing more on modulation rather than mere inhibition of inflammatory pathways.
Furthermore, the technology employed in the study exemplifies the interdisciplinary nature of modern neuroscience research. Utilizing genetic mouse models, advanced imaging techniques, and molecular assays, researchers were able to delineate the complex cellular interactions occurring during an inflammatory response, thus propelling forward the frontiers of our understanding.
In conclusion, Ngo et al.’s groundbreaking study has significantly contributed to the literature on neuroinflammation and astrocytic dynamics in genetically predisposed models of Parkinson’s Disease. The elucidation of how short-term inflammatory treatment activates astrocytes without leading to dopaminergic neuron loss opens new avenues for research and therapeutic exploration. As neuroscientists strive to uncover the underlying mechanisms of neurodegeneration, the interplay of inflammation and neuroprotection remains a critical frontier that warrants further exploration—a challenge that this study importantly underscores.
Subject of Research: Neuroinflammation and Astrocyte Activation in Parkinson’s Disease
Article Title: Short-term lipopolysaccharide treatment leads to astrocyte activation in LRRK2 G2019S knock-in mice without loss of dopaminergic neurons.
Article References:
Ngo, H.K.C., Srivastava, A., Le, H. et al. Short-term lipopolysaccharide treatment leads to astrocyte activation in LRRK2 G2019S knock-in mice without loss of dopaminergic neurons.
BMC Neurosci 26, 19 (2025). https://doi.org/10.1186/s12868-025-00939-7
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12868-025-00939-7
Keywords: astrocytes, neuroinflammation, LRRK2, Parkinson’s Disease, lipopolysaccharide, neuroprotection, GFAP, chronic inflammation, signaling pathways.