Recent advancements in the field of genetics and metabolomics have uncovered intriguing insights into the differences between male and female biological systems, particularly as they pertain to drug metabolism and deficiencies linked to the UDP-glucuronosyltransferase (UGT) enzyme family. A groundbreaking study led by Rivera-Herrera and colleagues has examined the sexual dimorphism exhibited in the metabolomic and phenotypic spectra of UGT deficiency, yielding pivotal findings from the Canadian Longitudinal Study on Aging. This study harnessed large-scale, population-based data to elucidate the complexities underpinning how gender may influence the metabolomic profiles of individuals and their physiological responses.
At the core of this research is the concept of UGT enzymes, which play a critical role in the phase II metabolism of numerous xenobiotics and endobiotics. By facilitating the conjugation of hydrophilic moieties to lipophilic substances, UGTs aid in the detoxification and excretion processes of various compounds from the human body. However, the expression and functionality of these enzymes can vary substantially between sexes. The implications of such variations extend beyond basic science and into clinical applications, especially considering the increasing recognition of personalized medicine’s relevance.
Utilizing data collected from a cohort spanning several years, underpinned by rigorous methodological frameworks, the researchers employed advanced metabolomics techniques to draw correlations between UGT deficiency markers and broader physiological trends. The study examined a multitude of metabolic pathways and biosynthetic routes influenced by sex, highlighting both commonalities and stark contrasts in how males and females metabolize drugs, hormones, and other biologically relevant substances.
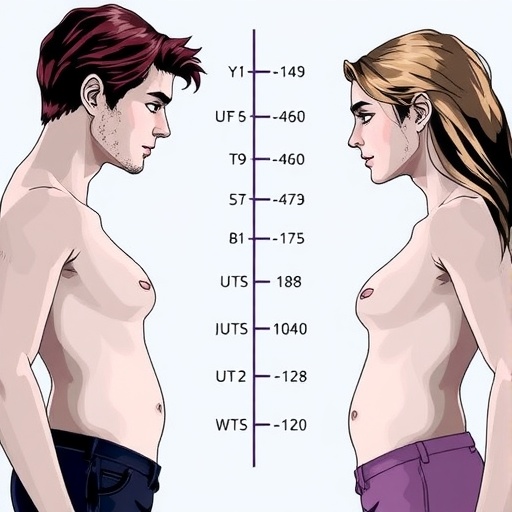
Notably, the findings suggest that the male and female bodies react differently to UGT deficiencies. In males, distinct metabolic pathways may converge into similar phenotypic outcomes, whereas females may experience broader fluctuations in metabolic profiles linked directly to UGT activity. This degree of sexual dimorphism sheds light on potential risks regarding drug interactions and adverse reactions in individuals with UGT deficiencies, which could inform future therapeutic interventions.
Furthermore, the study underscores the importance of gender-specific investigations in pharmacology and toxicology. By acknowledging the unique metabolic profiles exhibited by each sex, healthcare providers can tailor treatment regimens that minimize potential side effects and enhance therapeutic efficacy. Furthermore, these insights challenge the historically male-centric focus of clinical trials, emphasizing the necessity of inclusivity in research to avoid biases that could jeopardize women’s health.
As the implications of this research reverberate through the scientific community, the way forward calls for a more nuanced understanding of how biological sex influences metabolism and drug interaction outcomes. Future studies will be essential to dissect the underlying mechanisms responsible for these divergent pathways and further elucidate the molecular determinants driving UGT-related efficacy and safety in therapeutic contexts.
Intriguingly, the work of Rivera-Herrera and his team not only enriches existing knowledge but poses new questions regarding the genetic and environmental factors that contribute to the sexual dimorphism observed in UGT activity. By delving deeper into genetic variation and epigenetic modifications, researchers may uncover the layers of complexity that govern observable differences between sexes. This has the potential to transform approaches to treatment protocols and preventative health measures tailored to different demographics within the population.
Moreover, integrating metabolomic data with genomic information from larger biobanks could significantly enhance our understanding of the multifaceted interactions occurring between UGT enzymes and sex hormones, thereby informing more effective health strategies. As this field evolves, ongoing collaborative efforts among educators, researchers, and clinical practitioners will be essential in bridging gaps between laboratory findings and real-world medical practice.
The social implications of these findings cannot be overstated. As personalized medicine takes center stage, ensuring that both male and female patients receive appropriate care based on their unique metabolic profiles is paramount. The healthcare field must champion this transition by fostering awareness of gender-specific issues that can impact health outcomes and advocating for policies that prioritize inclusivity in research funding and clinical study designs.
In summary, this study enhances our understanding of the intricate relationship between sex and metabolic processes controlled by UGT enzymes. As we unravel the biological mechanisms that lead to differences in drug metabolism and potential toxicity, patients, healthcare providers, and researchers alike can feel empowered to create a future where gender-informed approaches to health and medicine become the norm.
Understanding these nuances will ultimately open doors to tailored therapies that lessen adverse drug reactions and mitigate the necessity for trial-and-error methodologies in prescription practices. As the conversation surrounding precision medicine grows, it becomes ever more critical to incorporate gender as a fundamental variable into research priorities.
The advancement of science is built upon the shoulders of rigorous investigation and peer-reviewed analysis. The entire academic community is challenged to expand its horizons in exploring how sexual dimorphism impacts not merely UGT deficiency but a wide array of health-related variables. Future inquiries could explore implications for various diseases, including but not limited to cancer, cardiovascular disease, and metabolic disorders, as they relate to gender-based biochemical responses.
In conclusion, Rivera-Herrera’s pioneering work serves as a compelling call to action for stakeholders across the spectrum—from laboratory researchers and clinical practitioners to policy-makers and patient advocates—to foster a health landscape that truly reflects the diverse needs of the population. By continuing to explore and understand the profound implications of sexual dimorphism in essential metabolic pathways, we can not only enhance science but also revolutionize the way we perceive healthcare.
Subject of Research: Sexual dimorphism in metabolomic and phenotypic spectra of UGT deficiency.
Article Title: Sexual dimorphism in metabolomic and phenotypic spectra of UGT deficiency: findings from the Canadian Longitudinal Study on Aging.
Article References:
Rivera-Herrera, A.L., Rouleau, M., Singbo, M. et al. Sexual dimorphism in metabolomic and phenotypic spectra of UGT deficiency: findings from the Canadian Longitudinal Study on Aging.
Biol Sex Differ 16, 26 (2025). https://doi.org/10.1186/s13293-025-00708-5
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s13293-025-00708-5
Keywords: UGT deficiency, sexual dimorphism, metabolomics, personalized medicine, drug metabolism, Canadian Longitudinal Study on Aging.