In a groundbreaking study published in Nature Communications, researchers have unveiled a pivotal role for the chromatin modifier SMC1A in the pathogenesis of systemic lupus erythematosus (SLE), a complex autoimmune disease characterized by widespread inflammation and multi-organ damage. This research elucidates how the sex-biased modulation of chromatin architecture by SMC1A shapes inflammatory responses, revealing a novel molecular axis that may underpin the disproportionate prevalence of SLE in females and offering promising therapeutic avenues.
SLE is a prototypic autoimmune disorder with a perplexing clinical heterogeneity and a marked female predominance, affecting approximately nine women for every man diagnosed. The molecular basis behind this sex bias has remained elusive, confounding efforts to develop targeted interventions. The present study addresses this gap by focusing on SMC1A, a structural maintenance of chromosomes protein involved in chromatin organization, which prior research has hinted might exert sex-dependent effects on gene regulation.
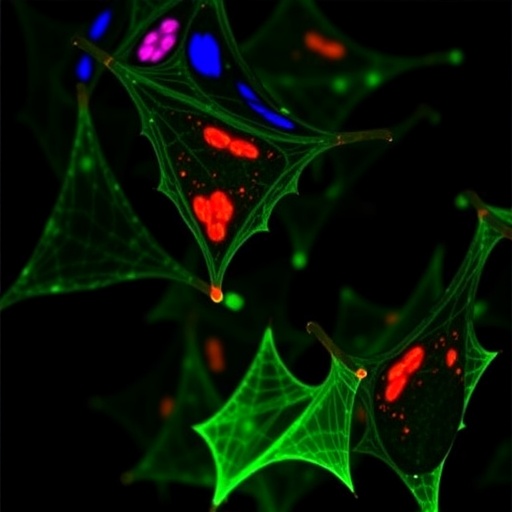
Chromatin remodeling plays an essential role in regulating gene expression by orchestrating how DNA is packaged within the nucleus. SMC1A is a core component of the cohesin complex that facilitates chromatin looping and higher-order structures fundamental for precise transcriptional control. By integrating epigenomic profiling, single-cell transcriptomics, and functional assays, the authors delineate how aberrant activity of SMC1A in immune cells influences gene networks associated with inflammation and autoimmunity.
The research team conducted comparative analyses of peripheral blood mononuclear cells (PBMCs) from patients with SLE and healthy controls, revealing that SMC1A expression is significantly upregulated in the former, particularly in females. This heightened SMC1A presence correlated with enhanced chromatin accessibility at promoter and enhancer regions of key inflammatory genes, illuminating a mechanistic link between sex-biased chromatin landscapes and proinflammatory transcriptional programs.
Using CRISPR-Cas9 mediated knockdown of SMC1A in lupus-prone immune cells, the investigators observed a marked attenuation in the expression of cytokines such as TNF-alpha, IL-6, and IFN-gamma, all central drivers of systemic inflammation. These data underscore the functional importance of SMC1A in orchestrating inflammatory cascades that perpetuate tissue damage in SLE. Furthermore, this repression mirrored a gain in repressive histone marks, indicative of a more compact chromatin state unfavorable for gene activation.
Intriguingly, the study identifies sex hormones as regulators of SMC1A expression and activity. Estrogen was found to enhance SMC1A-mediated chromatin remodeling, which might explain the heightened autoimmune susceptibility in females. This hormone-dependent modulation suggests that the interplay between hormonal milieu and chromatin modifiers could be a fundamental contributor to the sexual dimorphism observed in autoimmune diseases.
Another remarkable facet of the work lies in the integrative analysis of patient data, where high-resolution epigenetic maps linked SMC1A occupancy to loci implicated in genetic susceptibility to SLE. This convergence of genetic predisposition and epigenetic remodeling highlights the complex layers of regulation driving autoimmune pathogenesis. Such insights pave the way for personalized medicine approaches tailored to an individual’s chromatin state and sex-specific epigenetic signatures.
Beyond the fundamental discovery, the authors explored therapeutic implications by evaluating small-molecule inhibitors targeting components of the cohesin complex. Pharmacological inhibition of SMC1A function in murine lupus models led to amelioration of disease symptoms and reduced systemic inflammation, providing a proof-of-concept for targeting chromatin dynamics in autoimmune therapy. This represents a paradigm shift from conventional immunosuppression toward epigenetic modulation.
The study also probes the downstream signaling pathways influenced by SMC1A activity, revealing its impact on NF-κB and STAT signaling, two pivotal regulators of immune activation. By reshaping the chromatin accessibility landscape, SMC1A indirectly governs these pathways, amplifying inflammatory responses and fostering the auto-reactive immune milieu characteristic of SLE. Targeting such nodal points might yield more precise immunomodulatory effects with fewer off-target consequences.
Importantly, the research delineates how SMC1A dysregulation affects not only effector immune cells but also regulatory populations such as Tregs, which are critical for maintaining immune homeostasis. The compromised function of these cells in SLE pathogenesis may be partly attributable to altered chromatin states mediated by SMC1A, further elaborating on the multifaceted role of chromatin modifiers in orchestrating immune equilibrium.
This comprehensive study underscores the necessity of incorporating sex as a biological variable in biomedical research, particularly in autoimmune diseases where sex disparity is pronounced. It also emphasizes the emerging concept that chromatin architecture is a dynamic modulator of immune cell identity and function, directly influencing disease progression and therapeutic responsiveness.
Future directions highlighted by the authors include expanding the investigation to other chromatin remodelers with potential sex-biased activities and dissecting their combinatorial effects on the epigenome. Moreover, longitudinal studies tracking chromatin changes during disease flares and remissions may unravel dynamic regulatory mechanisms amenable to temporal therapeutic interventions.
In sum, this seminal work unravels a previously underappreciated layer of epigenetic regulation governed by the sex-biased chromatin modifier SMC1A, providing a mechanistic framework linking chromatin remodeling to autoimmune inflammation in SLE. By bridging fundamental chromatin biology with clinical immunology, it opens a promising frontier for developing sex-tailored epigenetic therapies that could revolutionize management strategies for systemic autoimmune diseases.
The implications of these findings extend beyond lupus, offering a conceptual blueprint for understanding how sex differences in chromatin regulation contribute to various immune-mediated disorders. As chromatin modifiers emerge as critical nodes integrating genetic, epigenetic, and environmental cues, their targeting holds exceptional promise for precision medicine tailored to the unique biological context of each patient.
This transformative research trajectory is poised to spark innovative clinical trials testing epigenetic drugs in SLE, potentially heralding a new era of therapeutic intervention that harnesses the plasticity of the epigenome to restore immune balance and prevent debilitating autoimmune damage.
Subject of Research: The sex-biased chromatin modifier SMC1A and its role in promoting autoimmunity in systemic lupus erythematosus (SLE).
Article Title: The sex-biased chromatin modifier SMC1A promotes autoimmunity by shaping inflammatory pathways in patients with SLE.
Article References:
Kosmara, D., Papanikolaou, S., Stathopoulou, C. et al. The sex-biased chromatin modifier SMC1A promotes autoimmunity by shaping inflammatory pathways in patients with SLE. Nat Commun 16, 10350 (2025). https://doi.org/10.1038/s41467-025-65309-7
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41467-025-65309-7