In a remarkable leap forward in the realm of dermatological diagnostics, researchers at Wake Forest University School of Medicine have unveiled a revolutionary wearable patch designed to detect skin cancer at its earliest stages with unprecedented accuracy and convenience. This battery-free, chip-less device promises to transform the way skin cancer screening is performed, especially benefiting populations with limited access to specialized dermatological care. By leveraging innovative bioimpedance measurement technology, the patch offers a non-invasive, objective, and user-friendly approach to monitoring cutaneous lesions, potentially saving countless lives through earlier intervention.
Skin cancer, particularly melanoma, remains one of the most lethal forms of cancer due to its capacity for rapid progression and metastasis. Early diagnosis is critical; however, traditional screening methods heavily depend on visual inspection, a process intrinsically subjective and prone to human error. Biopsies and sophisticated imaging, while more precise, are resource-intensive and confined to specialized clinical environments, creating a gap in accessibility. Addressing this challenge, the Wake Forest team set out to develop a tool that not only democratizes skin cancer detection but also enhances diagnostic fidelity through quantitative measurement.
At the core of this innovation lies bioimpedance, a technique that evaluates the electrical properties of biological tissues by measuring their resistance to alternating electrical currents. Malignant tissues exhibit distinct bioelectrical characteristics due to changes in cellular composition, water content, and membrane integrity. The new patch exploits these differences by employing safe electrical signals transmitted wirelessly to a reader device, enabling the precise interrogation of skin lesions’ physiological state without any physical or chemical intrusion.
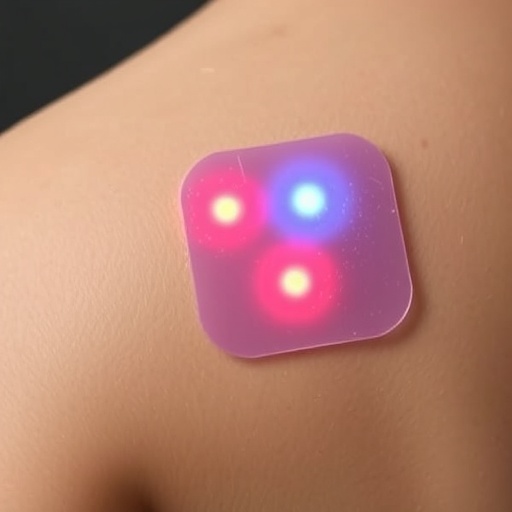
The device distinguishes itself by being entirely chip-free and batteryless, radically simplifying its design and use. Constructed as a thin, flexible patch, it adheres comfortably to the skin, conforming to its contours without impeding movement. Its lightweight nature and disposability also make it economically viable for widespread use. The absence of electronic circuitry and power sources reduces manufacturing costs and environmental impact while eliminating the need for maintenance or recharging, paving the way for routine home-based or primary care monitoring.
In a preliminary clinical evaluation, ten volunteers participated, each undergoing testing on both pigmented lesions and adjacent healthy skin. The patch measured bioimpedance across these regions, generating comprehensive electrical profiles that were analyzed statistically to confirm significant disparities between normal and potentially cancerous tissues. These results reveal the patch’s sensitivity in detecting abnormal lesions irrespective of the patient’s skin tone, highlighting its applicability across diverse populations—a critical factor in equitable health screening.
The technology’s ability to provide objective, quantitative data represents a paradigm shift from conventional visual assessments that rely heavily on expert interpretation. Numerical bioimpedance values can be tracked over time to monitor lesion evolution, offering clinicians actionable insights and potentially reducing unnecessary biopsies. This shift not only optimizes resource allocation but also minimizes patient anxiety and discomfort associated with invasive diagnostic procedures.
Importantly, the patch’s data-driven approach allows seamless integration with existing diagnostic workflows. It can complement imaging techniques and dermatological evaluations by adding a layer of electrical characterization that captures subtle tissue changes invisible to the naked eye or standard photographic methods. This multi-dimensional assessment enhances clinical decision-making, thereby improving early diagnosis and patient outcomes.
Another notable advantage is the patch’s privacy-preserving design. Unlike imaging-based diagnostics that capture identifiable visual data, bioimpedance measurements yield abstract numerical results, mitigating privacy concerns. This facilitates secure data storage and transmission, particularly pertinent for telemedicine applications where remote consultation is increasingly common.
The research team, led by Dr. Mohammad J. Moghimi, emphasizes the patch’s potential to empower both patients and healthcare providers. By making early detection tools accessible outside traditional clinical settings, this technology may substantially reduce the burden of late-stage skin cancer diagnoses, which often carry poorer prognoses and more intensive treatment requirements. Moreover, its affordability and ease of use position it as a scalable solution in public health initiatives aiming to curb skin cancer mortality.
Looking ahead, improvements are underway to enhance patch performance and patient comfort. Integration of conductive hydrogel electrodes is being explored to optimize skin contact and signal fidelity, further refining measurement accuracy. Additionally, larger clinical trials are planned to validate the patch’s diagnostic power across broader and more varied patient cohorts, including its ability to differentiate benign from malignant lesions conclusively.
This pioneering battery-free, chip-less patch marks a significant advance in medical technology, merging principles of bioengineering with pressing clinical needs. Its capacity to deliver rapid, non-invasive, and reliable skin cancer screening holds promise for transforming preventive care paradigms and saving lives through timely detection.
Subject of Research: People
Article Title: Wearable battery-free chip-less patch for bioimpedance measurement of cutaneous lesions
News Publication Date: October 22, 2025
Web References: https://www.nature.com/articles/s44385-025-00037-7
References: DOI 10.1038/s44385-025-00037-7
Image Credits: Wake Forest University School of Medicine
Keywords: Skin cancer, Cancer, Melanoma, Biomedical engineering, Medical technology