In a groundbreaking study recently published in Nature Communications, researchers have unveiled a novel molecular pathway implicating the RSAD2-YTHDF1 axis in the pathogenesis of inflammatory bowel disease (IBD). This discovery sheds unprecedented light on how smooth muscle cells (SMCs) contribute to intestinal inflammation by engaging in intercellular mitochondrial transfer, a mechanism previously underappreciated in gastrointestinal disease. The findings represent a paradigm shift, suggesting that beyond immune cells and epithelial barriers, the smooth muscle layer actively orchestrates inflammatory processes through intricate intracellular communications.
Inflammatory bowel disease, encompassing Crohn’s disease and ulcerative colitis, is characterized by chronic inflammation of the gastrointestinal tract, leading to debilitating symptoms and increased risk of colorectal cancer. While extensive research has focused on immune dysregulation and epithelial barrier dysfunction, the muscularis propria—the smooth muscle layer responsible for gut motility—has largely been considered a passive bystander in the inflammatory cascade. This new research overturns that notion by identifying functional molecular interactions within smooth muscle cells that exacerbate intestinal inflammation.
Central to this newly described pathway is RSAD2, also known as viperin, an interferon-inducible antiviral protein traditionally studied in the context of viral infections. The research team led by Zhang et al. demonstrate that RSAD2 expression is markedly upregulated in smooth muscle cells under inflammatory conditions. This upregulation is not merely a byproduct of inflammation but acts as a pivotal trigger that activates downstream effectors critical for disease progression.
One of the key downstream molecules identified is YTHDF1, an RNA-binding protein known for its role in recognizing N6-methyladenosine (m6A) modifications on mRNA—a prominent epitranscriptomic mark that regulates mRNA stability and translation. Zhang and colleagues reveal that RSAD2 physically interacts with YTHDF1, enhancing its expression and activity specifically within smooth muscle cells of the gut. This interaction orchestrates a complex post-transcriptional regulatory network that modulates mitochondrial dynamics and intercellular communication.
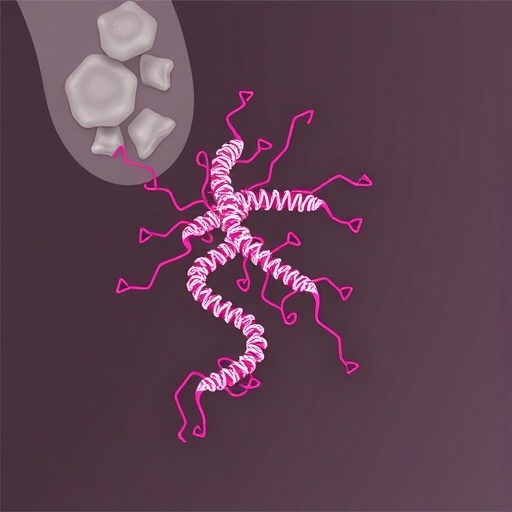
Mitochondria, the energy powerhouses of the cell, are well-known for their involvement in cellular metabolism and apoptosis. However, their role in inflammatory signaling has come into sharper focus recently, especially in the context of mitochondrial transfer between cells. This study provides compelling evidence that activated RSAD2-YTHDF1 signaling in smooth muscle initiates intercellular mitochondrial transfer to neighboring cells, including immune and epithelial cells. The transfer appears to be mediated via tunneling nanotubes or extracellular vesicles, enhancing the inflammatory milieu of the intestinal microenvironment.
Crucially, the mitochondria transferred possess altered bioenergetic profiles and elevated reactive oxygen species (ROS) production, which can aggravate cellular stress in recipient cells. This heightened oxidative environment stimulates the production of pro-inflammatory cytokines and chemokines, perpetuating a vicious cycle of inflammation. The discovery that smooth muscle cells act as active donors of dysfunctional mitochondria elucidates a novel intercellular communication axis contributing to chronic inflammation in IBD.
The ramifications of these findings extend beyond the mechanistic insights; they open the door for innovative therapeutic strategies. Targeting the RSAD2-YTHDF1 axis could selectively modulate mitochondrial transfer and dampen aberrant inflammatory signaling. The authors demonstrate that genetic knockdown or pharmacological inhibition of RSAD2 or YTHDF1 in smooth muscle cells significantly reduces mitochondrial transfer and ameliorates inflammation in murine models of IBD, underscoring the therapeutic potential.
Further molecular analyses reveal that YTHDF1’s role in this process hinges on its capacity to recognize m6A-modified transcripts encoding proteins that regulate mitochondrial trafficking and biogenesis. This epitranscriptomic regulation adds a sophisticated layer of control, linking RNA modifications to intercellular mitochondrial dynamics in a pathophysiological context. The integration of antiviral protein signaling with RNA modification machinery in smooth muscle cells epitomizes a novel intersection between metabolic regulation and immune control.
This study also highlights the importance of cell type-specific contributions to complex diseases like IBD. Traditionally, inflammation has been viewed predominantly through the lens of immune cells and barrier epithelial cells. The identification of smooth muscle as an active participant in fueling inflammation suggests the gut operates as an integrated organ system with dynamic cross-talk involving multiple cell types. The concept of smooth muscle cells as drivers of pathology introduces fresh perspectives on gut physiology and disease.
From a clinical standpoint, the potential to intervene in mitochondrial transfer mechanisms may herald a new class of treatments. Current therapies for IBD primarily target immune suppression or cytokine blockade, which can carry risks of systemic immunosuppression. Modulating the RSAD2-YTHDF1 axis offers a more localized approach, specifically attenuating pathological signaling emanating from smooth muscle cells, thereby minimizing off-target effects.
Moreover, the identification of mitochondrial transfer as a conduit for intercellular communication in gut inflammation invites exploration of similar pathways in other inflammatory and fibrotic diseases. Such cellular cross-talk via organelle transfer might represent a universal mechanism by which cells influence one another in tissue homeostasis and pathology. These broader implications warrant cross-disciplinary investigations, potentially catalyzing novel interventions across diverse clinical fields.
In addition to its translational relevance, the study contributes valuable methodological advancements. The team employed state-of-the-art imaging techniques to visualize mitochondrial transfer in real-time, coupled with sophisticated transcriptomic and epitranscriptomic analyses. Their combined approach enables precise dissection of molecular events driving complex cellular behaviors, setting a new benchmark for mechanistic research in inflammatory diseases.
The intricate interplay between RSAD2 and YTHDF1 uncovered by Zhang et al. also raises intriguing questions about the evolutionary roles of antiviral proteins beyond host defense. The repurposing of RSAD2 in smooth muscle cell-mediated inflammation introduces a new dimension to our understanding of innate immune proteins as modulators of tissue remodeling and intercellular signaling. This paradigm may inspire revisiting other antiviral factors for latent roles in chronic diseases.
While this research illuminates several critical aspects of smooth muscle biology and intestinal inflammation, it simultaneously underscores the complexity of IBD pathogenesis. The multifactorial nature of the disease demands a holistic perspective integrating genetic predisposition, environmental triggers, microbiota alterations, and now, smooth muscle cell signaling. Future studies will need to delineate how RSAD2-YTHDF1 activity integrates with these other factors to fully unravel IBD mechanisms.
In summary, the identification of the RSAD2-YTHDF1 axis as a driver of inflammatory bowel disease through intercellular mitochondrial transfer from smooth muscle cells revolutionizes our understanding of gut inflammation. This discovery marks a significant advance, charting new paths in both fundamental cell biology and clinical therapeutics. As we grapple with the rising global burden of IBD, such innovative molecular insights herald hope for more effective and targeted interventions to alleviate suffering and improve patient outcomes.
Subject of Research: The role of the RSAD2-YTHDF1 axis in smooth muscle cells in driving inflammatory bowel disease via intercellular mitochondrial transfer.
Article Title: Activation of the RSAD2-YTHDF1 axis in smooth muscle causes inflammatory bowel disease via intercellular mitochondrial transfer.
Article References:
Zhang, WD., Zhang, DD., Wang, X. et al. Activation of the RSAD2-YTHDF1 axis in smooth muscle causes inflammatory bowel disease via intercellular mitochondrial transfer. Nat Commun (2025). https://doi.org/10.1038/s41467-025-67707-3
Image Credits: AI Generated