Breast cancer remains one of the foremost global health challenges, accounting for a significant proportion of cancer-related deaths among women. The imperative for early and accurate detection continues to drive innovation in medical imaging, with strides in technology offering new rays of hope in improving diagnostic precision and patient outcomes. Recent breakthroughs in imaging modalities underscore a paradigm shift—moving beyond traditional mammography towards integrated, personalized approaches that cater to individual risk profiles and breast tissue characteristics.
Mammography, a century-honored cornerstone in breast cancer screening, has undergone remarkable evolution. The transition from analog to digital mammography revolutionized screening capabilities by enhancing image resolution and reducing radiation exposure significantly. The introduction of digital breast tomosynthesis, or 3D mammography, marks a critical advancement by mitigating the limitations of two-dimensional imaging, particularly tissue superimposition. This innovation provides three-dimensional reconstructions, elevating the cancer detection rate by up to 40% while decreasing false positives and recall rates, which historically burden patients with unnecessary anxiety and interventions.
Adding further nuance to mammographic imaging is contrast-enhanced spectral mammography (CESM), which leverages iodine-based contrast agents to illuminate tumor-associated vascularization. CESM mirrors magnetic resonance imaging (MRI) in its sensitivity to invasive lobular carcinomas and occult lesions, thereby bridging gaps where traditional mammography can falter. This hybrid approach enhances lesion conspicuity through differential x-ray photon absorption, ultimately refining diagnostic confidence and influencing clinical management.
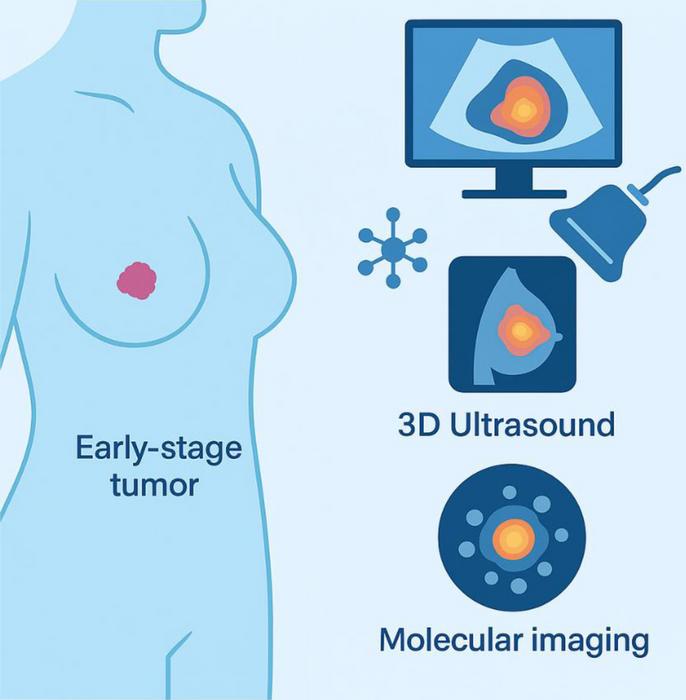
Ultrasound stands as an indispensable adjunct to mammography, particularly in women with dense breast tissue where mammographic sensitivity diminishes. Advances such as automated three-dimensional ultrasound have improved reproducibility and allowed for the detection of cancers otherwise elusive on mammograms. In parallel, contrast-enhanced ultrasound (CEUS) employs microbubble contrast agents to visualize microvascular flow dynamics within suspicious lesions, facilitating differentiation between benign and malignant masses. Such functional imaging modalities reduce reliance on biopsies and promote more precise clinical decisions.
Magnetic resonance imaging, long esteemed for its superior sensitivity—reportedly reaching 94% in high-risk cohorts—has established itself as the imaging modality of choice for BRCA mutation carriers and preoperative staging. The advent of high-field 3-Tesla MRI scanners significantly improves spatial resolution, granting clinicians unparalleled insight into tumor extent and multifocality. Nevertheless, limitations inherent to MRI, including cost, gadolinium contrast safety concerns, and a propensity for false-positive findings, require cautious use and continued refinement. Emerging abbreviated MRI protocols promise to mitigate some of these challenges by reducing scan time without sacrificing diagnostic accuracy.
Parallel to these established imaging techniques, burgeoning modalities are beginning to garner attention for their potential roles in breast cancer detection. Thermography, once sidelined due to limited specificity, has seen renewed interest through dynamic angiothermography (DATG), which detects thermoregulatory changes linked to neovascular growth. Although intriguing, this approach demands rigorous validation to establish clinical utility and standardization before widespread adoption. Similarly, molecular breast imaging (MBI), which uses radiotracers to highlight metabolic activity within tumors, shows promise in dense breast tissue but remains constrained by accessibility and cost considerations.
Positron emission tomography/computed tomography (PET/CT) remains predominantly a tool for staging advanced disease, owing to its metabolic imaging prowess but limited resolution for detecting sub-centimeter lesions. Its integration with MRI (PET-MRI) and the advent of optoacoustic imaging techniques hint at an exciting frontier where hybrid technologies might enable comprehensive structural and functional assessments simultaneously, optimizing early detection and treatment planning.
The establishment of risk-adapted screening protocols embodies the shift toward precision medicine in breast cancer care. Average-risk women are generally recommended biennial mammography starting between ages 40 and 50, balancing screening benefits against potential harms. Conversely, individuals at high genetic risk—such as BRCA mutation carriers—benefit from annual MRI supplemented by mammography commencing earlier in life. For women with dense breasts, supplemental ultrasound or tomosynthesis enhances detection rates that conventional mammography alone may miss, illustrating the demand for tailored strategies that transcend “one-size-fits-all” paradigms.
Despite technological triumphs, challenges remain. Healthcare disparities, radiation exposure concerns, and the risk of overdiagnosis represent persistent obstacles. Artificial intelligence (AI) integration emerges as a transformative solution, offering enhanced lesion detection algorithms and streamlining radiological workflows, which could democratize expert-level interpretation even in resource-limited settings. Coupling noninvasive biomarkers, such as liquid biopsies, with imaging techniques promises more nuanced stratification of malignancy risk and earlier intervention points.
Moreover, the quest for hybrid imaging approaches that synergistically combine molecular, anatomic, and functional data continues unabated. Innovations like PET-MRI and optoacoustic imaging aspire to revolutionize breast cancer detection by merging multiple diagnostic dimensions into single, comprehensive examinations. These next-generation techniques might ultimately facilitate precision-guided therapies, reducing unnecessary treatments and improving quality of life.
In conclusion, the landscape of breast cancer imaging is rapidly transforming through cutting-edge technological advances that prioritize early detection and patient-centric care. Mammography retains its foundational role, but its fusion with ultrasound, MRI, and emerging modalities creates a robust, multifaceted diagnostic arsenal. Future endeavors must focus on enhancing affordability, reducing radiation exposure, and establishing evidence-based personalized screening protocols to address global inequities. Multidisciplinary collaboration and continual innovation remain vital if we are to tilt the scales against breast cancer morbidity and mortality worldwide.
The promise of early breast cancer detection lies not only in machines and contrast agents but in synthesizing technological, biological, and clinical insights into cohesive screening programs. As imaging modalities continue to evolve, so too must our approach to integrating these tools, ensuring that each patient receives care tailored to her unique risk profile and clinical context. This vision for precision oncology heralds a new era in breast cancer diagnosis—one marked by smarter, safer, and more sensitive detection methods that ultimately save lives.
Subject of Research: Breast cancer imaging advancements and early detection techniques.
Article Title: Cutting-edge Imaging Breakthroughs for Early Breast Cancer Detection
News Publication Date: 30-Mar-2025
Web References:
https://www.xiahepublishing.com/journal/csp
http://dx.doi.org/10.14218/CSP.2024.00032
Image Credits: Ciro Comparetto, Franco Borruto
Keywords: Breast cancer, Mammography, Magnetic resonance imaging, Thermography, Medical diagnosis