A groundbreaking discovery from the Cancer Center at Illinois, led by Program Leader Erik Nelson, illuminates the intricate link between cholesterol metabolism and breast cancer progression, offering promising new avenues for therapeutic intervention. This research unravels previously uncharted molecular communication pathways that underpin breast cancer metastasis and therapy resistance, potentially reshaping future cancer treatment paradigms.
Breast cancer remains the second leading cause of cancer-related mortality among American women, with metastasis accounting for over 90% of fatalities. Despite advancements in therapeutic regimens, the complete landscape of molecular drivers fueling breast cancer dissemination and resistance to treatments has remained elusive. Nelson’s team has now made a pivotal contribution toward filling this critical knowledge gap by spotlighting the role of cholesterol metabolites in modulating tumor-immune interactions.
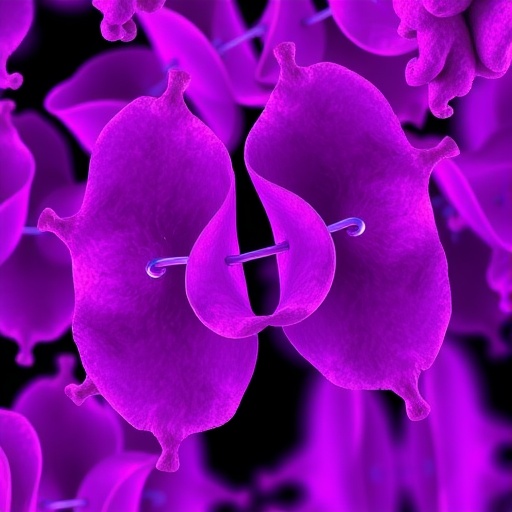
Building on prior epidemiological associations linking elevated cholesterol levels with adverse breast cancer outcomes, Nelson’s laboratory utilized sophisticated preclinical animal models to focus on a specific cholesterol derivative: 27-hydroxycholesterol (27HC). Their research delineates how 27HC orchestrates immune evasion mechanisms by modulating neutrophil behavior, fundamentally altering the immune system’s capacity to target and eliminate cancer cells. Neutrophils, a frontline immune cell subset, respond to 27HC by secreting extracellular vesicles (EVs), small membrane-bound particles that serve as potent intercellular communicators.
Delving deeper into the mechanistic underpinnings, the team uncovered that these neutrophil-derived EVs convey pro-tumorigenic signals to breast cancer cells, effectively reprogramming them toward a more aggressive phenotype. This communication axis actively promotes epithelial-mesenchymal transition (EMT), a cellular process where epithelial tumor cells acquire migratory, invasive, and stem-like characteristics, thereby enhancing metastatic potential and chemotherapy resistance. Such findings delineate how 27HC facilitates a microenvironment conducive to cancer progression by hijacking immune cell communication modalities.
The study, recently published in Cancer Letters, marks a significant advancement in our understanding of tumor-immune system crosstalk mediated through extracellular vesicles. First author Natalia Krawczynska elaborates on their discovery: “27HC instructs neutrophils to customize the cargo of secreted EVs, which subsequently interact with cancer cells, inducing transcriptional and phenotypic changes that endow them with stemness and chemoresistance.” These insights elevate the biological importance of EVs as not merely cellular debris but as sophisticated vehicles orchestrating cancer dynamics.
Erik Nelson emphasizes the translational potential of these findings: “By interrupting this neutrophil EV messaging system, we can sensitize metastatic breast cancer cells to existing chemotherapies, potentially improving patient outcomes.” This concept heralds a paradigm shift, suggesting that therapeutic strategies targeting EV-mediated communication could complement and potentiate current treatment modalities.
Looking forward, Nelson’s team aims to pioneer novel intervention strategies that disrupt the early-stage dialogue between neutrophil EVs and cancer cells. Early therapeutic blockade of this axis could reduce the incidence of metastatic spread, which remains the principal cause of breast cancer lethality. The laboratory plans to pursue high-throughput screening of available pharmacological agents and collaborate with chemists to engineer new compounds capable of modulating EV biogenesis and cargo composition.
Furthermore, the lab is exploring the influence of diet, pharmacological agents, and host biological factors on the neutrophil EV signaling network. Understanding how lifestyle and systemic variables impact this microenvironmental conversation could reveal adjunctive modalities to prevent cancer progression. The researchers also hypothesize that neutrophil EVs might exert multifaceted effects on other stromal and immune constituents within the tumor microenvironment, propagating a complex ‘telephone game’ of signals that collectively drive malignancy.
This multi-pronged research endeavor leverages the interdisciplinary expertise converging at the Cancer Center at Illinois, uniting biologists, bioengineers, chemists, and computational scientists in pursuit of comprehensive elucidation and therapeutic targeting of EV-mediated communication. The center’s collaborative ethos and technological resources position it uniquely to translate these molecular insights into clinical innovations.
In addition to preclinical exploration, Nelson’s lab is setting the stage for clinical collaborations aimed at evaluating the prognostic potential of circulating neutrophil EVs in breast cancer patients. Monitoring EV profiles in patient blood samples could serve as an early biomarker for metastatic relapse, enabling preemptive intervention strategies tailored to individual disease trajectories and enhancing personalized medicine approaches.
Crucially, the team demonstrated that neutralizing the ‘message’ encoded by 27HC-exposed neutrophil EVs can reverse the malignant phenotype, restoring sensitivity to chemotherapy and reducing metastatic competency. This proof-of-concept establishes a tangible target for future drug development and clinical trials, highlighting the therapeutic viability of disrupting immune cell-tumor communication vectors.
The implications of this research extend beyond breast cancer, as EVs are emerging as universal mediators in various cancer types and immune-related diseases. These findings not only deepen our molecular understanding of cancer biology but also inspire a novel class of interventions harnessing the modulation of immune-derived extracellular vesicles to combat metastasis and therapeutic resistance.
Overall, Erik Nelson and his colleagues have unveiled a sophisticated molecular mechanism by which a cholesterol metabolite manipulates immune surveillance to exacerbate breast cancer progression. Their work bridges fundamental immunology, cancer biology, and translational research, providing a foundation for innovative strategies to undermine tumor resilience and improve patient prognosis in the ongoing battle against breast cancer.
Subject of Research: The molecular mechanisms by which cholesterol metabolites, particularly 27-hydroxycholesterol (27HC), influence neutrophil extracellular vesicle secretion and the subsequent promotion of epithelial-mesenchymal transition and stemness in breast cancer cells, leading to enhanced metastasis and chemotherapy resistance.
Article Title: Neutrophils exposed to a cholesterol metabolite secrete extracellular vesicles that promote epithelial-mesenchymal transition and stemness in breast cancer cells
News Publication Date: 28 October 2025
Web References:
https://www.sciencedirect.com/science/article/pii/S0304383525006779
http://dx.doi.org/10.1016/j.canlet.2025.218105
Keywords: Cancer, Breast cancer, Metastasis