A new comprehensive study published in BMC Psychiatry offers a critical insight into the pervasive issue of relapse among psychiatric patients across Africa. This systematic review and meta-analysis aggregates data from multiple observational studies to unveil the alarming prevalence of relapse in mental health disorders within the continent. With mental illness recurrence rates soaring up to 60%, this scholarly work underscores the urgent need for enhanced intervention strategies tailored to the African context, revealing critical factors that contribute to the cycle of relapse.
Relapse in psychiatry is broadly defined as the deterioration or reappearance of symptoms after partial or complete recovery from a mental disorder. This condition poses a formidable challenge to clinicians, affecting long-term treatment efficacy and patients’ quality of life. The systematic review meticulously combines evidence from sixteen studies encompassing 4,660 African patients, providing a panoramic view of relapse dynamics seldom encapsulated in previous research focused on this geographically and culturally diverse population.
The analysis reveals that across the reviewed studies, the pooled relapse rate is estimated at 60.66%, a staggering figure indicating that nearly two-thirds of psychiatric patients face a return of debilitating symptoms. This high prevalence not only complicates the prognosis but also exacerbates the social and economic burdens on both patients and healthcare systems alike. The data amplify the critical necessity for mental health practitioners to prioritize relapse prevention in their treatment plans rigorously.
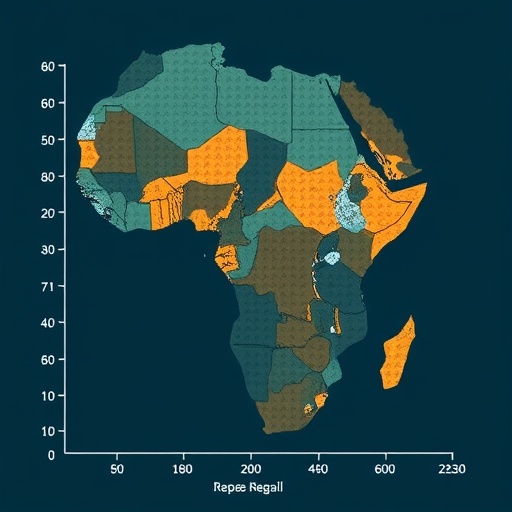
Geographical disparities were also prominent in the study, with the southern region of Africa exhibiting the highest relapse rate at 74.05%, and the eastern region showing a comparatively lower rate of 56.08%. This gradient highlights how regional variations—possibly influenced by differing healthcare infrastructures, sociocultural factors, and resource availability—affect relapse outcomes. Understanding these subtleties is paramount to developing region-specific health policies and tailored clinical practices.
One of the unequivocally identified drivers of relapse is medication non-adherence. The study presents a robust association between patients failing to adhere to prescribed psychiatric medication regimens and the likelihood of relapse, quantified by an adjusted odds ratio (AOR) of 3.09. This finding aligns with global psychiatric literature, reaffirming that adherence to pharmacological treatment is a cornerstone for sustaining remission and preventing symptom resurgence in chronic mental health conditions.
In addition to medication non-adherence, comorbidity of mental illnesses significantly increases the risk of relapse, carrying an adjusted odds ratio of 2.45. Patients grappling with multiple psychiatric conditions simultaneously face compounded vulnerabilities that challenge both diagnosis and treatment efficacy. This factor elevates the complexity of managing mental health disorders and calls for integrated care models that can address multifaceted clinical profiles.
The methodology employed in this meta-analysis ensured rigor and reliability by sourcing studies from extensive databases, including PubMed, African Journals Online, ScienceDirect, and EMBASE. The adoption of stringent inclusion criteria and the usage of advanced statistical tools like funnel plots and Egger regression tests minimized biases and strengthened the validity of the findings. Such methodological precision is critical in research domains where heterogeneous study designs often yield conflicting results.
Beyond raw statistics, the review illuminates a vital narrative about mental health care delivery challenges in Africa. Limited access to mental health services, stigma surrounding psychiatric disorders, and socio-economic hardships prevalent in many communities collectively contribute to treatment discontinuities and subsequent relapse. These systemic issues underscore the importance of policy-level interventions aimed at enhancing service accessibility and patient education.
The research also carries substantial implications for clinical practice. Mental health professionals are urged to intensify communication efforts with patients and their caregivers regarding the risks and signs of relapse. By fostering a collaborative care environment that addresses medication adherence and comorbidity management, clinicians can proactively mitigate relapse risks, potentially improving long-term outcomes and reducing the personal and societal toll of psychiatric disorders.
In light of these findings, the study advocates for prioritized investment in relapse prevention programs within mental health services. Targeted interventions, including adherence counseling, psychoeducation, and integrated treatment for comorbid conditions, are necessary components of comprehensive care frameworks. These strategies would not only improve patient outcomes but also be cost-effective by reducing rehospitalizations and chronic disability.
Future research directions emerging from this meta-analysis include exploring the socio-cultural determinants of medication adherence and relapse, examining the effectiveness of specific intervention models in diverse African settings, and longitudinal studies to track relapse trajectories over time. Addressing these gaps would further refine intervention design and promote sustainable mental health improvements.
While the study’s robust analytical approach ensures significant contributions to psychiatric epidemiology in Africa, it also highlights the persistent need for high-quality data. Many African nations face challenges in mental health data collection and surveillance, hampering efforts to form a full picture of relapse burdens and intervention impacts. Strengthening mental health research infrastructure is thus a parallel priority.
Ultimately, this meta-analysis serves as a compelling call to action for healthcare providers, policymakers, and researchers invested in the mental wellbeing of African populations. By spotlighting relapse prevalence and its determinants, the study enables informed decision-making and lays the foundation for evidence-based transformations in mental health care delivery across the continent.
Subject of Research: Relapse rates and associated factors among psychiatric patients in Africa
Article Title: Relapse and associated factors among psychiatric patients in Africa: a systematic review and meta-analysis
Article References:
Birhan, B., Rtbey, G. & Gelaw, K.A. Relapse and associated factors among psychiatric patients in Africa: a systematic review and meta-analysis. BMC Psychiatry 25, 333 (2025). https://doi.org/10.1186/s12888-025-06759-7
Image Credits: AI Generated