In a significant advancement for cancer treatment, researchers at the University of Arizona have unveiled a revolutionary method to enhance the delivery of chemotherapy drugs to pancreatic and breast cancer tumors with increased efficacy and reduced collateral damage to healthy tissues. This innovative approach, detailed in a paper recently published in Nature Cancer, focuses on reengineering the widely used chemotherapy agent paclitaxel, aiming to overcome its long-standing limitations related to toxicity and poor targeting.
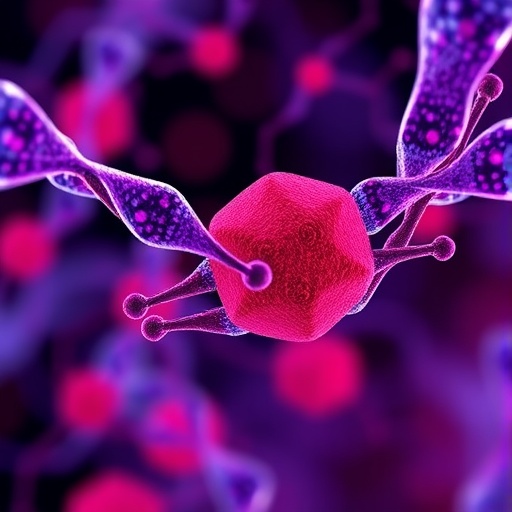
Paclitaxel, a cornerstone in chemotherapy regimens for various malignancies including breast, pancreatic, lung, and ovarian cancers, has historically posed challenges due to its nonspecific biodistribution. Upon administration, the drug often accumulates in non-target organs such as the liver and spleen, leading to severe side effects that limit dosing and jeopardize patient quality of life. The University of Arizona team, led by Dr. Jianqin Lu, developed a novel formulation that chemically conjugates paclitaxel to sphingomyelin, a naturally occurring sphingolipid abundant in cell membranes. This conjugation facilitates the self-assembly of the drug into nanovesicles—spherical structures on the nanometer scale surrounded by a lipid bilayer—thereby fundamentally altering its pharmacokinetics and biodistribution.
These nanovesicles, dubbed “Paclitaxome,” exhibit enhanced tumor targeting and extended systemic circulation. The underlying mechanism is multifaceted: the lipid-based nature of the nanovesicles enables them to evade rapid clearance by the mononuclear phagocyte system, while their size and surface chemistry promote preferential extravasation into tumor microenvironments through the enhanced permeability and retention (EPR) effect. As a result, Paclitaxome accumulates more densely within tumor tissues compared to free paclitaxel formulations, such as Taxol and Abraxane, minimizing systemic exposure and potential side effects.
Preclinical studies conducted in murine models of triple-negative breast cancer and advanced pancreatic cancer demonstrated that Paclitaxome significantly outperformed existing paclitaxel therapies. Tumor growth was markedly suppressed, and survival was extended in treated animals. By further engineering this platform—specifically incorporating a CD47-targeting peptide and an additional chemical modification named AZE—the team created an improved nanovesicle formulation (CD47p/AZE-Paclitaxome) that not only reduced tumor progression but also prolonged survival to a degree surpassing initial iterations.
One of the compelling aspects of this technology is its versatility in delivering combination therapies. By encapsulating gemcitabine, another frontline chemotherapeutic agent for pancreatic cancer, inside the nanovesicle core alongside paclitaxel on the outer lipid surface, the researchers achieved synergistic effects superior to simply co-administering both drugs separately. This co-delivery system enables precise control over drug ratios and release kinetics, potentially mitigating the systemic toxicity that often accompanies combination chemotherapy.
The therapeutic potential of this platform extends even further. In studies targeting triple-negative breast cancer recurrence, the research team combined the optimized paclitaxel nanovesicles with carboplatin, achieving notable prevention of tumor relapse and eradication of metastatic sites. These findings suggest that the nanovesicle system could serve as a modular drug delivery vehicle, tailored for diverse chemotherapeutic regimens and cancer types.
Beyond cancer, the researchers have demonstrated the adaptability of their nanovesicle approach. Application to camptothecin, a chemotherapy drug used in colon cancer, yielded promising results in preclinical colon cancer models. This broad-spectrum utility underscores the potential for this drug delivery technology to revolutionize treatment paradigms across multiple oncologic indications and possibly other diseases requiring targeted drug delivery.
Dr. Jianqin Lu envisions further integration of this nanovesicle platform with emerging immunotherapies to harness the body’s own defenses against malignancy. By co-delivering chemotherapeutic agents with immune-modulating therapeutics, there is the promise of not only direct cytotoxic effects but also the stimulation of durable antitumor immune responses. Current efforts in the laboratory are focused on deepening mechanistic insights and generating additional preclinical data to pave the way for first-in-human clinical trials.
Oncologist and study co-author Dr. Aaron Scott emphasizes that the prolonged systemic retention and targeted delivery conferred by Paclitaxome could significantly improve the therapeutic index of chemotherapy, a critical advancement for patients with cancers that currently have limited treatment options. The platform’s ability to maintain efficacious drug levels within tumors while minimizing adverse effects aligns with the overarching goal of precision oncology.
The study represents a collaborative effort bringing together experts in pharmaceutical sciences, oncology, molecular biology, and engineering from the University of Arizona. Their multidisciplinary approach was instrumental in translating fundamental insights about lipid biochemistry and nanotechnology into a tangible therapeutic candidate with demonstrable efficacy in animal models.
Funding for this pioneering research was provided by prestigious entities including the National Cancer Institute and the National Institute of General Medical Sciences, divisions of the National Institutes of Health, underscoring the significance and promise of the work. As the research community anticipates the transition of this technology into clinical phases, there is growing excitement about the impact it may have on improving survival outcomes and quality of life for cancer patients worldwide.
This landmark advancement highlights the power of nanomedicine in overcoming classical drug delivery hurdles. By leveraging the interface of chemistry, cell biology, and materials science, the University of Arizona team has opened new avenues for enhancing the efficacy of well-established chemotherapy agents, offering hope for more effective and safer cancer therapies in the near future.
Subject of Research: Animals
Article Title: A sphingolipid-derived paclitaxel nanovesicle enhances efficacy of combination therapies in triple-negative breast cancer and pancreatic cancer
News Publication Date: 21-Aug-2025
Web References:
10.1038/s43018-025-01029-7
References:
Lu J, Wang Z, Li W, Jiang Y, Li M, Wu S, Ma T, Tran TB, Cordova LE, Erdrich J, Schroeder J, Lin E, Scott A. A sphingolipid-derived paclitaxel nanovesicle enhances efficacy of combination therapies in triple-negative breast cancer and pancreatic cancer. Nature Cancer. 2025.
Keywords: Cancer treatments, chemotherapy, nanovesicles, paclitaxel, pancreatic cancer, breast cancer, drug delivery, nanomedicine, combination therapies