In an innovative leap forward for cancer treatment monitoring, researchers have unveiled a sophisticated approach to assess bone alterations in prostate and rectal cancer patients undergoing helical tomotherapy (HT). This technique leverages megavoltage computed tomography (MVCT) imaging to capture dynamic changes in the femoral head and neck regions, utilizing radiomic feature analysis to detect subtle variations induced by radiotherapy. The study promises a new frontier in personalized cancer therapy, where real-time monitoring of bone tissue response could inform treatment adjustments and improve patient outcomes.
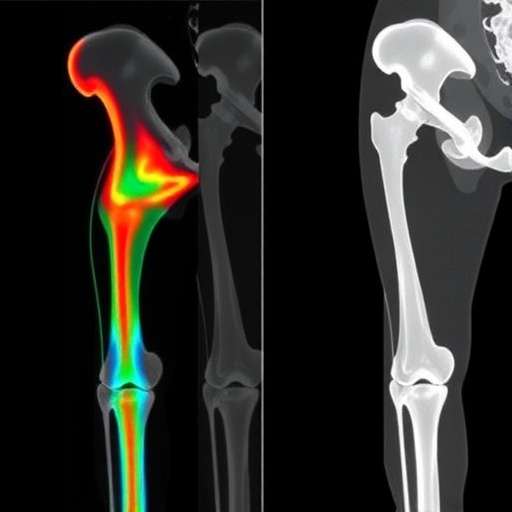
Radiomics—the extraction of high-dimensional quantitative features from medical images—has been gaining traction as a powerful tool to decode the complex biological response to cancer therapy. Central to this study is the application of radiomic analysis specifically focused on the femoral head and neck bones in patients treated with HT, a form of intensity-modulated radiation therapy renowned for its precision and conformal dose delivery. By systematically evaluating radiomic features (RFs) over the course of treatment, the research addresses critical gaps in understanding how bone tissue structurally adapts or deteriorates in response to radiation.
The investigative team conducted their analysis on a cohort of 20 male patients, equally divided between prostate cancer (PCa) and rectal cancer (RCa). MVCT imaging datasets were acquired at three key time points—baseline, midpoint, and treatment conclusion—allowing for longitudinal tracking of radiomic feature changes. The femoral regions of interest were meticulously segmented, ensuring accurate capture of tissue morphology and texture attributes within these bone structures.
A hallmark of this study was the stringent reproducibility assessment performed using a cheese phantom to identify robust RFs. This step was pivotal for eliminating features susceptible to scanner noise or imaging artifacts, thereby ensuring that subsequent analyses reflected true biological variations rather than technical confounders. Such rigor in feature selection underpins the reliability of correlations drawn between RF alterations and radiation dose distributions.
Analytical methodologies employed included repeated measures analysis of variance (ANOVA) to characterize absolute and relative percentage changes in RF values throughout the radiation course. Furthermore, the Pearson correlation coefficient adjusted by the Benjamini-Hochberg procedure was utilized to statistically validate associations between radiomic shifts and administered radiation dose, setting a conservative false discovery rate threshold (q < 0.05).
Results revealed that the most striking variations occurred in intensity-histogram (IH) and intensity-based (IB) radiomic features within the femoral head and neck regions. These RF families encapsulate fundamental properties such as tissue density distribution and grayscale variability, serving as sensitive indicators of microarchitectural bone changes that may elude conventional radiological assessment. Complementing these, texture-based RFs derived from gray-level co-occurrence matrix (GLCM) analyses illuminated heterogeneity patterns likely linked to radiation-induced bone remodeling.
A remarkable discovery was the strong inverse correlation (correlation coefficient approximately -0.7) between RF changes in PCa patients’ femoral regions and the delivered radiation dose. This suggests that higher radiation doses induced measurable, dose-dependent alterations in bone tissue characteristics captured through radiomics. In rectal cancer patients, correlations were somewhat more nuanced. Noteworthy correlations emerged for IB features such as the coefficient of variation in the femoral neck and for IH features like the minimum histogram gradient and robust mean absolute deviation in the femoral head. These findings illustrate that specific RFs are sensitive to dose-related changes across different anatomical subregions and cancer types.
The temporal dimension uncovered that mid-treatment and treatment-end RF variations correlated distinctly with dose fractionation schemes. This temporal sensitivity hints at the capacity of radiomic surveillance to function as an early biomarker, flagging bone tissue response ahead of overt radiological or clinical manifestations. Consequently, the translational potential of incorporating RF monitoring into routine clinical workflows is profound, potentially enabling adaptive radiotherapy where dosing regimens are tailored according to real-time tissue response.
These insights fundamentally enrich the current paradigm of oncology imaging by highlighting the utility of MVCT beyond its traditional role in patient positioning. Radiation oncologists and medical physicists now have at their disposal a non-invasive, objective, and quantifiable mean to monitor subclinical bone health, fostering timely interventions that could mitigate radiation-associated bone toxicity, fractures, or necrosis.
Moreover, the study underscores the value of IB, IH, and GLCM-based features as pivotal RF candidates warranting further validation in larger cohorts. This sets the stage for multi-institutional studies and prospective clinical trials aimed at refining radiomic signatures predictive of bone resilience or susceptibility under radiotherapeutic stress.
Overall, this breakthrough spotlights radiomics as a critical enabler of precision medicine, empowering clinicians to visualize and quantify tissue-level effects with unprecedented granularity. The capacity to detect early bone alterations could revolutionize supportive care strategies, reduce complications, and ultimately enhance the therapeutic ratio in cancer radiotherapy.
As HT continues to be widely adopted for pelvic malignancies, integrating radiomic monitoring protocols could standardize patient-specific risk stratification and management. Such integration promises to transcend conventional imaging assessments limited to structural changes, progressing toward a holistic understanding of tissue microenvironment alterations induced by radiation.
Future research avenues may explore correlating these radiomic biomarkers with clinical endpoints such as fracture incidence, pain scores, and functional mobility metrics, thereby elucidating their prognostic significance. Additionally, expanding analysis to other bony anatomical sites susceptible to irradiation could generalize applicability across diverse oncologic contexts.
In conclusion, the study presents compelling evidence that robust radiomic features derived from MVCT in helical tomotherapy exhibit meaningful, dose-related variations in the femoral head and neck during prostate and rectal cancer treatment. These findings herald a paradigm shift in oncologic imaging, positioning radiomics as a vital tool for the early detection and dynamic tracking of bone tissue changes, ultimately fostering more personalized and adaptive radiation therapy strategies.
Subject of Research: Analysis of radiomic feature changes in the femoral head and neck during helical tomotherapy in prostate and rectal cancer patients.
Article Title: Variations in radiomic features of the femoral head and neck during helical tomotherapy in prostate and rectal cancer patients.
Article References:
Gholizade, M., Yazdani, E., Hosseini-Baharanchi, F.S. et al. Variations in radiomic features of the femoral head and neck during helical tomotherapy in prostate and rectal cancer patients. BMC Cancer 25, 1509 (2025). https://doi.org/10.1186/s12885-025-14903-5
Image Credits: Scienmag.com