First-in-Human Trial Highlights Breakthrough DLL3-Targeted Therapy for Relapsed Small Cell Lung Cancer
In a landmark development in the treatment of relapsed small cell lung cancer (SCLC), scientists have unveiled promising results from the first-in-human Phase 1 clinical trial of SHR-4849, a novel antibody-drug conjugate (ADC) that selectively targets Delta-like ligand 3 (DLL3) expressed on tumor cells. Presented at the 2025 World Conference on Lung Cancer, this study signifies a potential paradigm shift for SCLC patients, a group long plagued by limited therapeutic options and dismal prognoses.
Small cell lung cancer, an aggressive malignancy accounting for roughly 10% to 12% of lung cancer cases globally, is notorious for its rapid growth, early metastasis, and poor response to conventional therapies. Despite intensive research, therapeutic breakthroughs have remained elusive, primarily because of the tumor’s molecular complexity and rapid development of resistance. DLL3, an inhibitory Notch pathway ligand aberrantly expressed on the surface of SCLC cells but largely absent in normal adult tissues, has emerged over the past decade as a highly attractive therapeutic target. By exploiting this tumor-specific expression, targeted agents like SHR-4849 aim to deliver potent cytotoxic payloads directly to cancer cells while sparing healthy tissues, thereby enhancing efficacy and minimizing systemic toxicities.
SHR-4849 is a sophisticated biotherapeutic composed of a humanized anti-DLL3 IgG1 monoclonal antibody linked via a cleavable linker to a potent DNA topoisomerase I inhibitor. Topoisomerase I inhibitors interfere with the DNA replication process by stabilizing the transient DNA-enzyme complexes during replication progression, which ultimately induces double-strand breaks and triggers cancer cell death. The conjugation of this toxin to the antibody allows precise delivery to DLL3-expressing tumor cells, releasing the cytotoxic agent intracellularly after internalization via receptor-mediated endocytosis. This mechanism offers a promising way to strike SCLC cells specifically, limiting collateral damage to normal cells.
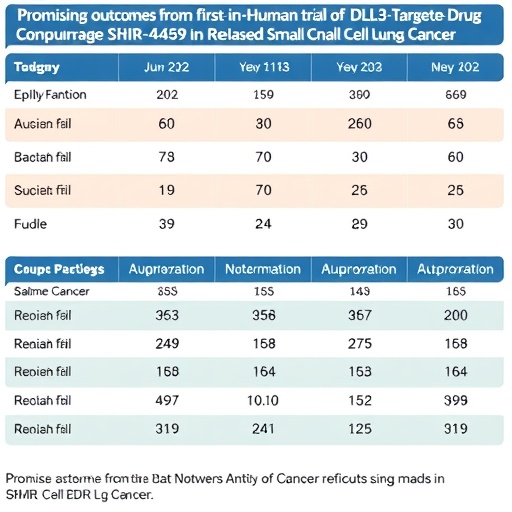
The multi-center Phase 1 clinical study, led by Dr. Linlin Wang and colleagues at the Affiliated Cancer Hospital of Shandong First Medical University, enrolled 54 patients with relapsed SCLC who had limited treatment options. The trial employed an adaptive dose-escalation and expansion design, assessing SHR-4849 across five predetermined dose levels ranging from 0.8 to 4.2 mg/kg. The primary objectives were to evaluate the safety profile, determine the maximum tolerated dose, establish the pharmacokinetic characteristics, and observe preliminary antitumor activity in this heavily pretreated patient population.
Remarkably, among the 42 patients evaluable for response, SHR-4849 achieved an objective response rate (ORR) of 59.5%, a noteworthy figure in the context of relapsed SCLC where typical response rates for current therapies often linger below 30%. The disease control rate (DCR), encompassing patients achieving stable disease or better, reached an impressive 90.5%, signaling durable tumor stabilization. Notably, a subset of patients with at least 12 weeks of follow-up demonstrated an even higher ORR of 69.2%, while the expansion cohort receiving 2.4 mg/kg exhibited responses in nearly 78% of participants. These efficacy signals are particularly compelling given the aggressive nature of relapsed SCLC and underscore SHR-4849’s potential as a transformative agent.
Safety and tolerability remain paramount in oncology drug development, and SHR-4849 demonstrated a manageable safety profile. The most frequently recorded treatment-related adverse events included hematologic toxicities such as decreased white blood cell counts, anemia, and neutropenia, along with common gastrointestinal symptoms including nausea. Importantly, no treatment-related adverse events necessitated permanent discontinuation or led to patient mortality. Furthermore, no dose-limiting toxicities were seen below the highest tested dose of 4.2 mg/kg, reinforcing the drug’s favorable therapeutic window.
Pharmacokinetic assessments revealed consistently low plasma concentrations of the free toxin across all dose levels, indicating stable linker integrity and controlled release of the cytotoxic payload. This pharmacological behavior is critical because premature release of the toxin could lead to systemic toxicity, whereas targeted release inside tumor cells maximizes therapeutic effect. The study’s design, incorporating both dose escalation and expansion phases, is currently continuing to refine the recommended Phase 2 dose (RP2D) to balance maximal efficacy with minimal adverse effects.
These encouraging preliminary findings position SHR-4849 as an exciting candidate in the sparse landscape of SCLC therapeutics, particularly for the relapsed setting where options are severely restricted. The selective targeting of DLL3 exploits a tumor-specific vulnerability, potentially offering a precision medicine approach that overcomes some of the limitations inherent in conventional chemotherapies. Ongoing studies will further characterize SHR-4849’s efficacy and safety while exploring biomarkers that may predict patient response and aid in personalized treatment strategies.
Dr. Wang emphasized the significance of these early data, stating, “Our encouraging results demonstrate the promise of DLL3-directed ADCs in addressing an unmet need for patients with relapsed SCLC. We look forward to advancing SHR-4849 through later-phase trials that will provide more definitive evidence of its clinical benefit.” The continued clinical development of SHR-4849 will include larger cohorts and potentially combination regimens to maximize antitumor activity.
These advancements arrive at a critical time, as lung cancer remains the leading cause of cancer mortality worldwide. According to the International Agency for Research on Cancer (IARC), lung cancer incidence in 2022 reached approximately 2.48 million cases globally, with small cell lung cancer comprising nearly one-tenth of these diagnoses. Despite being a less common subtype, SCLC accounts for a disproportionately high mortality rate due to its aggressive clinical course and limited treatment progress over recent decades.
The International Association for the Study of Lung Cancer (IASLC) has long championed research innovations aimed at improving lung cancer outcomes. The 2025 World Conference on Lung Cancer served as an ideal platform to unveil these pivotal findings, reflecting the worldwide collaborative efforts to tackle thoracic malignancies through cutting-edge science and clinical trials. With nearly 7,000 participants, the conference fosters dissemination of breakthroughs like SHR-4849, which could redefine therapeutic paradigms.
In summary, the first-in-human study of SHR-4849 heralds a new chapter in SCLC treatment, combining targeted molecular therapy with an antibody-drug conjugate design that promises substantial tumor control with manageable safety. While additional clinical data are awaited, the early efficacy signals and tolerability profile fuel optimism that this agent may soon become a vital weapon against this devastating disease. As researchers continue to refine dosing strategies and expand patient access, SHR-4849 exemplifies the power of precision oncology in transforming lung cancer care.
Subject of Research: DLL3-targeted antibody-drug conjugate therapy in relapsed small cell lung cancer
Article Title: First-in-Human Trial Shows Promising Results for DLL3-Targeted Antibody-Drug Conjugate SHR-4849 in Relapsed Small Cell Lung Cancer
News Publication Date: September 7, 2025
Web References: https://www.iarc.who.int/wp-content/uploads/2025/02/pr359_E.pdf?utm_source=chatgpt.com
Keywords: Lung cancer, Small cell lung cancer, DLL3, Antibody-drug conjugate, SHR-4849, Targeted therapy, Phase 1 clinical trial, Topoisomerase I inhibitor