In a groundbreaking study published in the Journal of Biomedical Science, researchers have unveiled compelling insights into the role of Protein Arginine Methyltransferase 5 (PRMT5) in cardiac health. This advancement stems from their efforts to delineate the mechanisms driving pressure overload-induced hypertrophy and heart failure. The implications of this research are significant, especially for individuals suffering from various cardiac conditions exacerbated by hypertrophy. The findings present a new dimension for understanding the intricacies of cardiac remodeling and its broader implications on heart function.
Hypertrophy, characterized by an increase in the size of heart muscles, is a prevalent response to pressure overload, commonly stemming from conditions such as hypertension or aortic stenosis. Chronic hypertrophy ultimately leads to heart failure, a condition that poses one of the most substantial public health burdens worldwide. Understanding the pathways that govern these processes is crucial for developing effective therapeutic strategies.
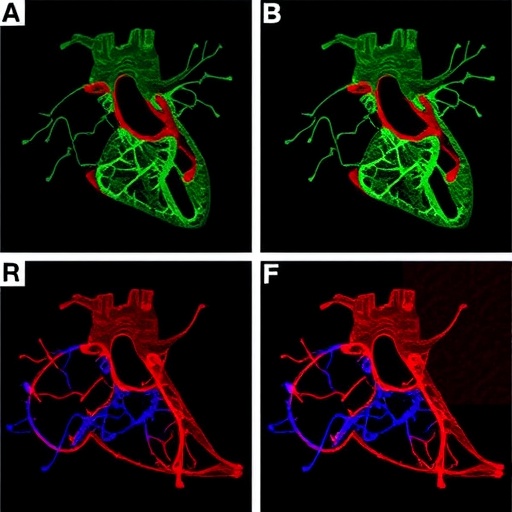
The study effectively highlights the differential role of PRMT5 by employing genetically modified mouse models. Researchers discovered that cardiac-specific overexpression of PRMT5 led to pronounced cardiac dilation and worsening heart function. This finding is particularly alarming as it suggests that higher levels of PRMT5 are decidedly detrimental in the context of cardiac stress. The implications of these observations could reshape how clinicians approach the management of hypertrophy and the potential for cardiac failure in affected patients.
Moreover, the study meticulously outlines the molecular mechanisms through which PRMT5 exerts its effects. It was observed that PRMT5 interacts with various proteins critical for maintaining cardiac function. This interaction results in a cascade of biochemical events that culminate in adverse cardiac remodeling. The ability to pinpoint specific interactions underscores the potential for targeted interventions aimed at mitigating PRMT5 activity as a therapeutic strategy.
Beyond the biochemical pathways, the researchers also scrutinized the influence of PRMT5 on gene expression within cardiomyocytes, the heart’s muscle cells. The overexpression of PRMT5 was linked to the upregulation of genes associated with hypertrophic signaling and fibrosis, which invariably lead to impaired cardiac function. The identification of this gene regulatory network lays the groundwork for investigating novel therapeutic targets that could reverse the deleterious effects of pressure overload.
As heart failure, particularly due to pressure overload-induced hypertrophy, presents a multifactorial problem, the study emphasizes the need for a comprehensive understanding of underlying molecular targets. PRMT5, once regarded as an enzyme with a largely peripheral role in cardiology, is now emerging as a significant contributor to heart disease pathology. This paradigm shift necessitates a reevaluation of existing treatment modalities, which have, until now, largely overlooked the implications of post-translational modifications in cardiomyocytes.
The research elucidates that the cardiac ramifications of PRMT5 extend beyond mere hypertrophy. The study’s findings indicate a pronounced increase in apoptosis within cardiomyocytes, emphasizing the enzyme’s role not just in hypertrophic signaling but also in cell survival pathways. This revelation is groundbreaking, as it suggests that strategies aimed at modulating PRMT5 levels could address not only hypertrophy but also prevent the loss of cardiomyocytes that often worsens heart failure prognosis.
Methodologically, the researchers employed a variety of advanced techniques, including RNA sequencing and mass spectrometry, to map the changes in cardiac tissue comprehensively. These analyses provided critical insights into the proteins and pathways that are influenced by PRMT5 overexpression. The meticulous approach underscores the robustness of their findings, paving the way for future investigations into pharmacological inhibitors that could selectively target PRMT5 activity in cardiac tissue.
In light of the findings, there is a pressing need to communicate these results effectively to the broader scientific community and public health stakeholders. This research not only advances our understanding of heart biology but also opens avenues for novel therapies that could dramatically enhance patient outcomes in hypertensive heart disease. The urgency of addressing heart failure, especially in an aging population, lends additional weight to the significance of this study.
As investigations continue, future studies are warranted to explore the potential of developing PRMT5 inhibitors as therapeutic agents. Such inhibitors could be a game changer in the clinical management of hypertrophic cardiomyopathy, thereby improving the quality of life for millions globally. The path forward involves a rigorous exploration of the safety and efficacy of these inhibitors in clinical settings.
Overall, the findings from Katanasaka and colleagues propel PRMT5 into the spotlight, challenging longstanding narratives surrounding cardiovascular disease and signaling a new era of therapeutic exploration. The intricate relationship between PRMT5 and cardiac hypertrophy and failure beckons further research, potentially leading to advancements in personalized medicine approaches for heart disease management.
In conclusion, the groundbreaking study elucidates critical pathways by which PRMT5 contributes to pressure overload-induced hypertrophy and subsequent heart failure. As researchers delve deeper into the mechanisms at play, the hope is to develop targeted therapies that could alleviate the clinical burdens associated with heart disease. The promising results from this research represent not just a leap forward in understanding fundamental cardiac biology but also a beacon of hope for innovative treatments that can ultimately improve patient care and outcomes.
Subject of Research: The role of PRMT5 in cardiac hypertrophy and heart failure.
Article Title: Correction: Cardiac-specific overexpression of PRMT5 exacerbates pressure overload-induced hypertrophy and heart failure.
Article References:
Katanasaka, Y., Sunagawa, Y., Sakurai, R. et al. Correction: Cardiac-specific overexpression of PRMT5 exacerbates pressure overload-induced hypertrophy and heart failure.
J Biomed Sci 32, 80 (2025). https://doi.org/10.1186/s12929-025-01174-2
Image Credits: AI Generated
DOI: 10.1186/s12929-025-01174-2
Keywords: PRMT5, cardiac hypertrophy, heart failure, pressure overload, cardiomyocytes, gene expression, therapeutic targets.