Balancing Maternal Mental Health and Child Development: The Complex Landscape of Prenatal SSRI Use
Pregnancy is a transformative period marked by profound physiological and psychological changes. For many women, this phase can be overshadowed by the onset or exacerbation of mood disorders such as depression and anxiety. These conditions not only affect the well-being of the expectant mother but also carry significant implications for child development and long-term health outcomes for both mother and offspring. The challenges of managing maternal mental health during pregnancy are compounded by the complexities involved in selecting appropriate treatment modalities, particularly when symptoms escalate beyond mild severity.
Selective serotonin reuptake inhibitors (SSRIs) have emerged as the most commonly prescribed class of antidepressants during pregnancy. SSRIs function by increasing serotonin levels in the brain, a neurotransmitter with critical roles in mood regulation and neurodevelopment. Their widespread use is predicated on their efficacy in ameliorating depressive and anxiety symptoms, thereby theoretically conferring benefits not only to mothers but also to their children through improved maternal health and environment. However, the story of SSRI use in pregnancy is far from straightforward and remains rife with scientific debate.
A growing body of research has sought to elucidate the developmental consequences of prenatal exposure to SSRIs. Some studies report associations with adverse neurobehavioral outcomes, including altered motor development, cognitive deficits, and increased risk for neuropsychiatric disorders later in life. These findings have generated considerable concern among clinicians and patients alike. Nevertheless, these conclusions are often complicated by methodological challenges, confounding variables, and a lack of consensus across studies.
One persistent conundrum lies in disentangling the effects of maternal mental illness itself from the pharmacological impact of SSRIs on the developing fetus. Untreated maternal depression and anxiety are independently linked to negative birth outcomes, such as preterm birth, low birth weight, and altered stress regulation in offspring. These adverse effects can have enduring consequences, setting trajectories for chronic health and behavioral disorders. Therefore, withholding effective treatment during pregnancy also carries significant risk.
The existing literature is further complicated by the diversity of environmental, genetic, and social factors that intersect to influence maternal mental health, treatment decisions, and child development. Socioeconomic status, quality of family relationships, exposure to discrimination, and access to healthcare resources all modulate the severity of maternal symptoms, the likelihood of receiving SSRIs, and subsequent developmental trajectories in offspring. These intersecting variables challenge simplistic causal interpretations and highlight the necessity for nuanced research methods.
Addressing these complexities requires methodological rigor and innovative conceptual frameworks. Traditional epidemiological designs often struggle to account for confounding by indication — the phenomenon where the underlying condition prompting treatment is itself a contributor to observed outcomes. Advanced techniques such as sibling comparison studies, propensity score matching, and the incorporation of genetic data (e.g., polygenic risk scores) hold promise for teasing apart these intertwined effects.
Moreover, longitudinal designs that track both maternal mental health and child developmental outcomes over extended periods can provide critical insights into temporal relationships and potential critical windows of vulnerability or resilience. Integrating biological measures, such as neuroimaging and biomarker analysis, may also clarify the mechanistic pathways through which antenatal SSRIs and maternal mood disorders exert their influences.
Conceptually, it is essential to move beyond a binary narrative that frames SSRI use during pregnancy solely in terms of risk. Instead, a balanced perspective that acknowledges potential benefits is warranted. Improved maternal mental health may enhance prenatal care adherence, nutrition, and the postnatal caregiving environment, all of which contribute to positive developmental outcomes. Thus, the decision to initiate or continue SSRI treatment during pregnancy entails weighing a complex calculus of risks and benefits, both pharmacological and psychosocial.
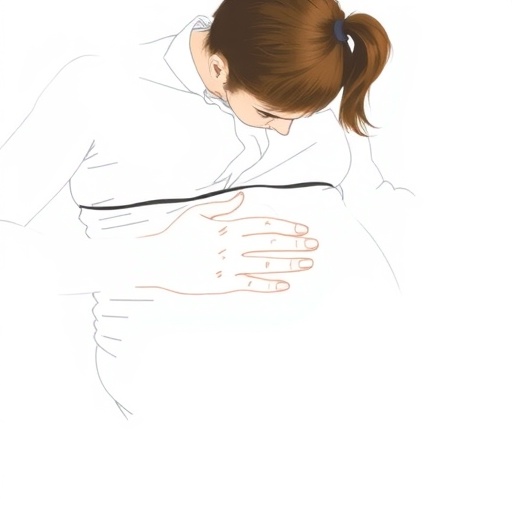
Clinicians face the formidable task of individualizing treatment plans within this uncertain landscape. Shared decision-making strategies that incorporate patient values, symptom severity, and current evidence can empower mothers while minimizing potential harms. Additionally, fostering multidisciplinary collaboration among obstetricians, psychiatrists, pediatricians, and social workers can create comprehensive support systems for pregnant women navigating mental health challenges.
Public health policies must also reflect the multifactorial reality of perinatal mental illness. Addressing social determinants of health, expanding access to mental health services, and reducing stigma surrounding antidepressant use during pregnancy are crucial steps. Furthermore, investing in research that embraces methodological sophistication and complexity will be instrumental in generating actionable knowledge.
In conclusion, prenatal SSRI use represents a paradigm at the intersection of maternal mental health, pharmacology, developmental neuroscience, and social context. Far from being a monolithic risk factor, SSRIs serve as tools whose impact depends on an array of intersecting influences. Future inquiry must embrace this complexity with robust study designs and integrative frameworks to unravel the true nature of SSRI treatment effects in pregnancy. This endeavor holds promise not only for advancing scientific understanding but also for guiding clinical care toward optimized outcomes for mothers and their children.
Subject of Research: Investigating the risks and benefits of prenatal selective serotonin reuptake inhibitor (SSRI) use on maternal mental health and child developmental outcomes.
Article Title: Potential risks and benefits of prenatal selective serotonin reuptake inhibitor medications for maternal mental health and child development
Article References:
Pawluski, J., Oberlander, T.F. Potential risks and benefits of prenatal selective serotonin reuptake inhibitor medications for maternal mental health and child development. Nat. Mental Health (2025). https://doi.org/10.1038/s44220-025-00480-w
Image Credits: AI Generated