In a groundbreaking study published in Nature Communications, researchers have unveiled the molecular underpinnings of the persistent nasal epithelium abnormalities observed in individuals suffering from post-COVID syndrome. Leveraging the cutting-edge single-cell RNA sequencing (scRNA-seq) technology, the team led by Reddy et al. has illuminated how inflammatory mediators, specifically TNFα and TGFβ, orchestrate aberrant epithelial differentiation that may perpetuate chronic symptoms months after acute SARS-CoV-2 infection. This discovery adds a critical piece to the complex puzzle of ‘long COVID,’ providing novel insights with potential therapeutic implications.
The study’s focus on the nasal epithelium is particularly significant given that the nasal passage serves as a primary entry and replication site for SARS-CoV-2. While much research has historically concentrated on pulmonary and systemic effects of COVID-19, the local tissue changes in the nasal mucosa and their contribution to long-term symptomatology have remained elusive. The investigators obtained nasal epithelial biopsies from post-COVID syndrome patients and employed scRNA-seq to interrogate the cellular composition and gene expression profiles at unprecedented resolution. This technique enabled the dissection of cellular heterogeneity and identification of cell states altered by the post-viral milieu.
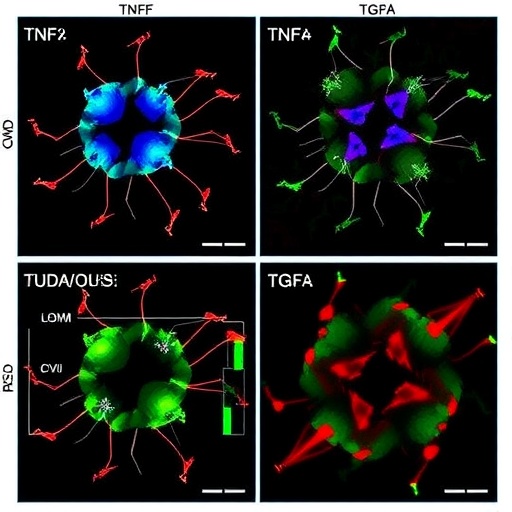
Their analyses revealed a striking persistence of abnormal epithelial cell differentiation patterns months following viral clearance. Specifically, they observed a skewing away from the normal ciliated cell fate—critical for mucociliary clearance—and a predilection towards a basal-like or squamous cell identity that compromises epithelial barrier function. Such aberrant cellular phenotypes likely underlie the chronic nasal congestion, anosmia, and mucosal inflammation reported by patients. Importantly, these alterations were not merely epiphenomena but appeared to be maintained by sustained upregulation of key inflammatory pathways.
Among the molecular culprits, tumor necrosis factor alpha (TNFα) and transforming growth factor beta (TGFβ) emerged as central players driving this aberrant differentiation program. Both cytokines are well known mediators of inflammation and tissue remodeling, often implicated in chronic respiratory diseases. Their persistent elevation in the nasal mucosa post-COVID suggests an inflammatory milieu that frustrates tissue homeostasis and regeneration. Functional experiments demonstrated that antagonizing TNFα and TGFβ signaling could partially restore normal epithelial differentiation trajectories, raising hope for targeted therapies.
These findings are remarkable in highlighting how the post-viral microenvironment can rewire cellular fate decisions in epithelial tissues long after the initial insult has resolved. The authors hypothesize that the interplay between inflammatory mediators and resident stem/progenitor cells leads to a pathological regeneration process that sustains disease symptoms. This paradigm shifts the therapeutic focus from merely combating viral infection to modulating chronic inflammation and tissue remodeling during recovery phases.
Additionally, the study employed advanced bioinformatics and trajectory inference algorithms to reconstruct the differentiation paths of nasal epithelial cells. This approach revealed bottlenecks and decision points where epithelial cells deviate from canonical pathways, potentially offering biomarkers to stratify patients and monitor treatment responses. The integration of single-cell transcriptomics with spatial mapping technologies further mapped the cellular architecture disrupted in post-COVID mucosa, offering a spatial context to the transcriptional abnormalities.
The implications of this work extend beyond post-COVID syndrome. Similar mechanisms of aberrant epithelial regeneration driven by inflammatory cytokines could underlie other chronic respiratory conditions such as chronic rhinosinusitis and asthma. Thus, the insights gained may provide broader frameworks for understanding epithelial dysfunction in diverse pathologies. Moreover, this research underscores the importance of longitudinal tissue sampling and molecular profiling in deciphering post-infectious sequelae—a frontier area in precision medicine.
Clinically, the persistence of epithelial dysfunction may partly explain why many patients continue to suffer from respiratory symptoms, fatigue, and impaired olfaction months to years after COVID-19. Current treatments are largely symptomatic and nonspecific. By pinpointing TNFα and TGFβ as key drivers, this study paves the way for clinical trials targeting these pathways using existing biologics or novel inhibitors aimed at restoring proper epithelial repair mechanisms.
The robustness of these findings stems from a well-curated patient cohort and rigorous methodological design. The authors accounted for confounders such as age, co-morbidities, and initial disease severity, strengthening the generalizability of the conclusions. Moreover, parallel in vitro models of nasal epithelial differentiation corroborated in vivo observations, demonstrating that cytokine exposure modulates differentiation in a cell-intrinsic manner. These complementary approaches consolidate the causative role of inflammatory pathways in post-COVID epithelial abnormalities.
Despite the compelling data, the study acknowledges remaining questions. For instance, the temporal dynamics of TNFα and TGFβ elevation during recovery phases remain to be fully delineated. It is also unclear why some individuals develop persistent epithelial dysregulation while others recover fully, pointing to potential genetic or environmental modifiers. Future investigations expanding sample size and including diverse populations will be crucial to unravel these complexities.
This work also spotlights the transformative power of single-cell genomics in infectious disease research. The granular insight into cellular states and trajectories enabled by scRNA-seq offers unprecedented windows into tissue biology affected by viral infections. As the technology matures, integrating multi-omic datasets may further elucidate epigenetic and metabolic reprogramming underlying long COVID and other post-infectious syndromes.
Personalized medicine approaches may emerge from findings such as these, wherein patients with identified cytokine-driven epithelial derangements receive tailored anti-inflammatory regimens. Early intervention during the convalescence phase might prevent the establishment of chronic epithelial remodeling, altering the natural history of post-COVID syndrome. Additionally, nasal epithelium biopsies combined with molecular profiling could serve as diagnostic tools in clinical practice.
Taken together, this landmark study by Reddy and colleagues delivers vital insights into the pathophysiology of post-COVID syndrome, revealing how persistent inflammation commandeers nasal epithelial differentiation. By delineating the contributions of TNFα and TGFβ, the research not only deciphers molecular mechanisms but also charts potential therapeutic avenues. As the global healthcare community grapples with the long-term burden of COVID-19, such mechanistic understandings will be indispensable for devising effective treatments and improving patient outcomes.
As we continue to unlock the mysteries of post-viral syndromes, the integration of single-cell technologies promises to revolutionize our ability to define disease at cellular resolution and tailor interventions accordingly. This study exemplifies the confluence of innovative science and clinical relevance—a beacon of hope for millions enduring the lingering shadows of COVID-19.
Subject of Research:
Persistent aberrant differentiation in nasal epithelium driven by inflammatory cytokines in post-COVID syndrome.
Article Title:
scRNA-seq reveals persistent aberrant differentiation of nasal epithelium driven by TNFα and TGFβ in post-COVID syndrome
Article References:
Reddy, K.D., Maluje, Y., Ott, F. et al. scRNA-seq reveals persistent aberrant differentiation of nasal epithelium driven by TNFα and TGFβ in post-COVID syndrome. Nat Commun 16, 9494 (2025). https://doi.org/10.1038/s41467-025-64778-0
Image Credits: AI Generated