In a groundbreaking new study that could reshape therapeutic approaches for pancreatic cancer, researchers have revealed a compelling synergy between PLK1 inhibition and the chemotherapeutic agent gemcitabine. This combination appears to significantly enhance apoptotic mechanisms within pancreatic cancer cells, offering renewed hope in the fight against one of the deadliest malignancies. The study, published in Medical Oncology, meticulously dissects the molecular crosstalk between critical signaling pathways, uncovering how PLK1’s suppression modulates downstream effectors to potentiate cell death. The implications run deep, suggesting a paradigm shift in chemotherapeutic regimens and furnishing a fresh molecular map for future drug development.
Pancreatic cancer notoriously resists conventional therapies, partly due to its intricate survival signaling networks that thwart apoptosis, the programmed cell death that typically curtails aberrant cell proliferation. Traditional chemotherapy, such as gemcitabine—long-established as a frontline treatment—often grapples with limited efficacy due to intrinsic or acquired resistance. The current investigation addresses this critical barrier by elucidating how targeted inhibition of Polo-Like Kinase 1 (PLK1), a pivotal regulator of cell cycle progression and mitosis, can sensitize pancreatic cancer cells to gemcitabine’s apoptotic triggers. This finding is pivotal, as PLK1 is frequently overexpressed in aggressive tumors and tied to poor prognosis.
At the cellular and molecular level, PLK1 exerts intricate control over multiple checkpoints during mitotic entry and progression, ensuring genomic stability and cell division fidelity. The new research reveals that abrogation of PLK1 activity disturbs these tightly regulated processes, precipitating a cascade that weakens cancer cells’ defense systems. The utilization of small-molecule inhibitors to suppress PLK1 demonstrated a marked increase in gemcitabine-induced apoptosis when administered together, compared to either agent alone. This synergy underscores a previously underappreciated nexus between cell cycle control and apoptotic machinery.
Crucially, the study highlights the dual modulation of two major signaling axes: the ERK1/2-Bim pathway and the AKT1-Noxa axis. ERK1/2, part of the mitogen-activated protein kinase (MAPK) pathway, plays a paradoxical role in cancer, either promoting survival or death depending on context. Here, PLK1 inhibition was found to potentiate ERK1/2 activation in a manner that elevates Bim—a pro-apoptotic Bcl-2 family member known for its pivotal role in mitochondrial apoptotic signaling. The upregulation of Bim facilitates the release of cytochrome c from mitochondria, triggering the caspase cascade and culminating in cell death.
Simultaneously, the study delineates how PLK1 inhibition hampers AKT1 signaling, a well-characterized pro-survival kinase whose hyperactivation is commonly linked to chemoresistance and malignant progression. Reduced AKT1 activity results in the enhanced expression of Noxa, another pro-apoptotic BH3-only protein. Noxa contributes to apoptosis by neutralizing anti-apoptotic proteins such as Mcl-1, further tipping the balance toward cell demise. This complementary effect between the ERK1/2-Bim and AKT1-Noxa axes crafts a potent molecular milieu favoring apoptosis, explaining the amplified efficacy of gemcitabine when co-administered with PLK1 inhibitors.
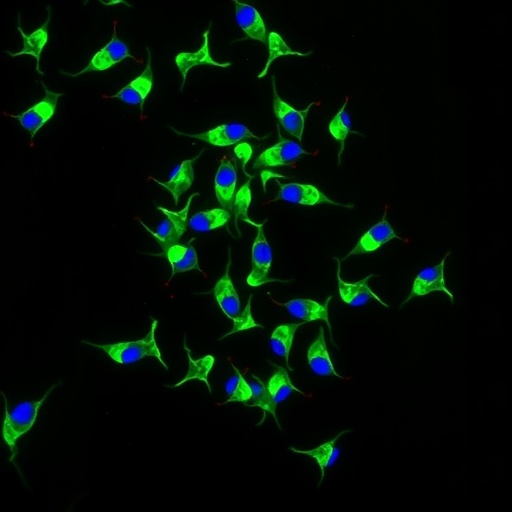
Importantly, these insights were not merely deduced from computational modeling or indirect biochemical assays but substantiated through rigorous in vitro experiments in pancreatic cancer cell lines. The researchers employed a blend of Western blot analyses, flow cytometry for apoptosis quantification, and cell viability assays to provide a comprehensive picture of the interactive dynamics. The results were consistently robust across multiple experimental conditions, reinforcing the validity of the proposed mechanistic model.
Moreover, the work gestures toward exciting translational potential. Given that PLK1 inhibitors are already in various stages of clinical development for other malignancies, their repurposing or combination with gemcitabine therapy in pancreatic cancer appears both feasible and promising. By circumventing conventional resistance mechanisms, this combinatorial approach could extend patient survival and improve quality of life—a critical aim where therapeutic options remain limited and prognosis remains bleak.
The study’s implications extend beyond the laboratory bench. They ignite a broader conversation about the strategic targeting of cell cycle regulators in synergy with chemotherapy, a paradigm that could reverberate across oncology. It challenges the dogmatic reliance on broad-spectrum cytotoxic agents, advocating instead for precision-guided modulation of cancer cell vulnerabilities. The delineation of the ERK1/2-Bim and AKT1-Noxa signaling as key mediators also invites further exploration, beckoning researchers to unravel deeper layers of apoptotic regulation and inter-pathway crosstalk.
Another noteworthy aspect is the potential for biomarker development. If ERK1/2-Bim and AKT1-Noxa signatures can be reliably detected and quantified in patient-derived tumors, they may function as predictive indicators for response to combined PLK1 inhibition and gemcitabine treatment. Such biomarkers would empower oncologists to tailor therapies with heightened precision, optimizing efficacy while minimizing unnecessary toxicity.
The study also opens avenues to investigate resistance mechanisms that may emerge against this combination therapy. Cancer cells notoriously adapt, and understanding how they might bypass PLK1 inhibition or modulate ERK1/2 and AKT1 pathways could preempt therapeutic failure. This knowledge will be critical for designing next-generation inhibitors or adjunct therapies to sustain treatment responses.
Furthermore, the role of the tumor microenvironment in influencing PLK1 and apoptotic signaling dynamics should not be overlooked. The interplay between cancer cells and their surrounding stroma, immune infiltrates, and extracellular matrix components profoundly impacts drug sensitivity. Integrating this contextual complexity into future research will be vital for translating these molecular insights into clinical realities.
In sum, this study illuminates a transformative strategy harnessing PLK1 inhibition to amplify gemcitabine-induced apoptosis in pancreatic cancer cells through sophisticated modulation of ERK1/2-Bim and AKT1-Noxa signaling pathways. It exemplifies how molecular precision and combinatorial therapeutics can converge to challenge one of the most formidable cancers affecting humanity. As this research moves from bench to bedside, it holds the promise of reshaping treatment paradigms and rekindling hope for patients confronting pancreatic cancer’s grim prognosis.
Subject of Research:
Pancreatic cancer; Molecular mechanisms of PLK1 inhibition and gemcitabine-induced apoptosis; ERK1/2-Bim and AKT1-Noxa signaling pathways.
Article Title:
PLK1 inhibition enhances gemcitabine-induced apoptosis through PLK1-dependent ERK1/2-Bim and AKT1/Noxa signals in pancreatic cancer cells.
Article References:
Lu, B., Li, H., Deng, D. et al. PLK1 inhibition enhances gemcitabine-induced apoptosis through PLK1-dependent ERK1/2-Bim and AKT1/Noxa signals in pancreatic cancer cells. Med Oncol 42, 508 (2025). https://doi.org/10.1007/s12032-025-03062-z
Image Credits: AI Generated