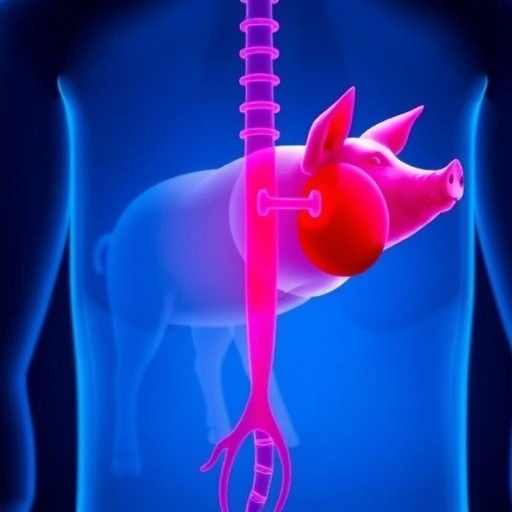
In a landmark advancement addressing the global shortage of transplantable kidneys, researchers have successfully demonstrated the viability of genetically modified pig kidneys in a human recipient for an unprecedented 61-day period. This breakthrough xenotransplantation was performed on a brain-dead human recipient who had undergone nephrectomy, marking a pivotal moment in the quest to alleviate organ scarcity for patients suffering from end-stage renal disease.
The transplant utilized pig kidneys from alpha-Gal knockout pigs, genetically engineered to eliminate a key antigen responsible for triggering hyperacute rejection in xenotransplantation. Unlike prior highly modified grafts that incorporated multiple genetic alterations and aggressive immunosuppression regimens, this study employed kidneys with minimal genetic modification and clinically approved immunosuppressive drugs, notably without CD40 pathway blockade. These deliberate methodological choices aimed to emulate more realistic clinical conditions and assess the intrinsic capabilities of such modified organs.
Post-transplant, the pig kidneys supported hemodynamic stability and electrolyte balance, ultimately liberating the recipient from dialysis dependence. Such findings highlight the capacity of xenografts from gene-edited pigs to sustain essential renal functions in a human physiological environment, laying a foundation for future therapeutic applications beyond experimental models.
Initial histopathological analyses on postoperative day 10 revealed unique immunological responses within the transplanted graft. There was prominent glomerular deposition of IgM and IgA antibodies alongside activation of early complement components and evidence of mesangiolysis—a pattern not typical of traditional allotransplant rejection. Remarkably, these changes occurred in the context of stable renal function without proteinuria, suggesting a distinct immunological milieu characterizing pig-to-human xenotransplantation.
However, by postoperative day 33, serum creatinine levels acutely elevated, signaling impending graft dysfunction. This biochemical indicator coincided with clinical and histological hallmarks of antibody-mediated rejection, including an increase in donor-specific IgG antibodies. These immunological developments prompted the clinical team to initiate therapeutic interventions targeting the antibody-mediated alloimmune response.
A combination therapy involving plasma exchange, C3/C3b complement inhibition, and rabbit anti-thymocyte globulin (rATG) proved efficacious, completely reversing the rejection episode. This multimodal approach underscores the complexity of managing xenogeneic immune responses and the potential necessity of integrating complement inhibition and lymphocyte-depleting strategies to maintain graft viability.
In-depth immunologic monitoring revealed expansion and activation of pre-existing donor-reactive T cell clones circulating in the recipient. These T cells progressively acquired an effector phenotype with transcriptional profiles characteristic of immune activation. At the time of rejection, these alloreactive clones were detected within the graft itself prior to the administration of rATG, implicating them as central mediators in the immunopathogenesis of xenograft failure.
This study is the first to provide comprehensive long-term monitoring encompassing physiological performance, immunologic dynamics, and infectious risk in a pig-to-human kidney transplant setting. The findings reveal that, despite significant immunosuppressive efforts, pre-existing xenoreactive T cells combined with antibodies targeting currently unidentified epitopes remain formidable barriers to sustained xenograft survival.
The transplantation’s success in providing life-supporting renal function for over two months substantiates the promise of minimally gene-edited pig organs. This proof-of-concept paves the way for refinement of genetic engineering techniques and immunomodulatory protocols to achieve durable graft acceptance without the extensive alterations previously deemed necessary.
With escalating global demand for donor kidneys and the persistent organ shortage crisis, xenotransplantation from genetically engineered pigs offers a tangible solution. The insights gleaned from this human cadaveric model facilitate the translation of findings into clinical trials and eventual therapeutic reality, fostering hope for thousands on transplant waitlists.
The implications of this research extend beyond nephrology, potentially informing xenotransplant strategies for other organ systems plagued by donor scarcity. As scientists decode the intricate interplay between human immune defenses and porcine graft antigens, novel targets for intervention and improved graft designs will emerge.
While ethical, regulatory, and infectious safety considerations accompany this promising frontier, the demonstrated feasibility of pig-to-human kidney transplantation propels the field toward tangible clinical application. Future efforts will focus on mitigating immune rejection, optimizing gene editing, and ensuring long-term graft function—goals essential for xenotransplantation to become a mainstream therapeutic option.
The publication of these findings in a prestigious scientific journal underscores the transformative potential of xenotransplantation to revolutionize organ transplantation. It heralds a new era where interspecies organ sharing may effectively address the unmet demands of patients with irreversible organ failure, reshaping transplantation medicine in profound ways.
Subject of Research:
Article Title:
Article References:
Montgomery, R.A., Stern, J.M., Fathi, F. et al. Physiology and immunology of pig-to-human decedent kidney xenotransplant. Nature (2025). https://doi.org/10.1038/s41586-025-09847-6
Image Credits: AI Generated