In a groundbreaking study poised to reshape our understanding of psychiatric disorders, researchers have unveiled a novel pharmacological approach that rescues social impairments in rats engineered to manifest the pathological hallmarks of Disrupted-in-Schizophrenia-1 (DISC1) protein aggregation. This seminal work, anticipated to be published in the forthcoming 2026 issue of Schizophrenia, leverages cutting-edge molecular neuroscience techniques to address the elusive biological underpinnings of schizophrenia’s social deficits, offering fresh hope for therapeutic interventions targeting this devastating symptom cluster.
DISC1, a scaffold protein essential for proper neuronal development and synaptic functioning, has long stood at the center of schizophrenia research due to its genetic linkage and mechanistic involvement in neural circuitry disorders. Previous studies have demonstrated how aberrations in DISC1 folding and aggregation disrupt intracellular signaling and synaptic plasticity, culminating in the cognitive and social dysfunctions characteristic of major psychiatric illnesses. Yet, translating these molecular insights into effective treatments has remained a formidable challenge. The current investigation surmounts this obstacle by employing a pharmacological agent that mitigates DISC1 aggregation, thereby restoring the integrity of neural networks responsible for social behavior.
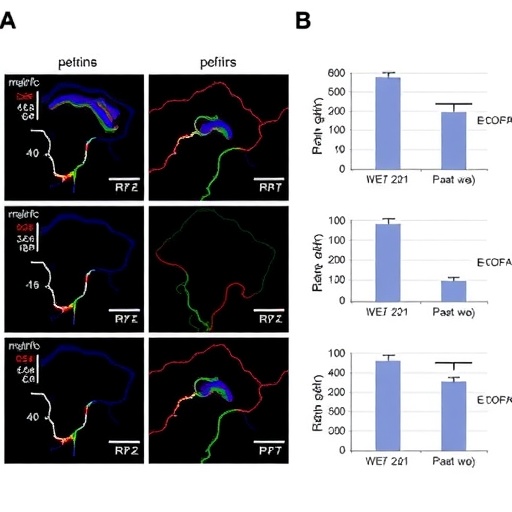
Central to the study’s methodology was the generation of a rat model genetically engineered to exhibit pathological accumulation of misfolded DISC1 protein, recapitulating the proteinopathy seen in a subset of schizophrenia patients. These transgenic rats faithfully displayed pronounced social withdrawal, diminished social interaction times, and aberrant ultrasonic vocalizations—behavioral phenotypes mirroring core deficits observed in human schizophrenia. The researchers subjected these animals to a precision pharmacological regimen designed to target the aggregation-prone domain of DISC1, effectively preventing oligomer formation without disrupting its physiological roles.
The pharmacological agent’s action is rooted in its capacity to stabilize the native conformation of the DISC1 protein, obviating the misfolded intermediates that seed toxic aggregates. Structural biology analyses revealed that the drug binds selectively to hydrophobic patches exposed during early misfolding events, thereby enhancing proteostasis mechanisms such as chaperone-mediated autophagy and ubiquitin-proteasome degradation. This multimodal modulation underscored a profound neuroprotective effect, reinstating normal synaptic receptor distribution and reestablishing excitatory-inhibitory balance within prefrontal cortical circuits implicated in social cognition.
Behavioral assessments conducted following acute and chronic administrations of the compound demonstrated remarkable normalization of social interaction metrics. Notably, treated DISC1-aggregate rats exhibited increased time spent in social engagement zones, heightened reciprocal interactions, and restoration of social communication signals, as quantified by nuanced ethological monitoring and advanced machine learning-based behavior recognition algorithms. The improvements extended beyond mere symptomatic relief; electrophysiological recordings highlighted a resumption of synchrony within key brain oscillations, particularly gamma rhythms critical for cognitive integration.
Importantly, the therapeutic intervention showed resilience across developmental windows, ameliorating social impairments both when administered during adolescence—a critical period for schizophrenia onset—and in mature adult animals displaying fully manifested pathology. This finding suggests a versatile window for clinical applicability and addresses longstanding questions about the reversibility of neurodevelopmental disruptions. Complementary transcriptomic analyses of treated cortical tissue revealed upregulation of genes associated with synaptic remodeling, neurogenesis, and inflammatory resolution, delineating a broad spectrum of molecular remediation triggered by DISC1 stabilization.
The implications of this research transcend the immediate context of DISC1 pathology, shedding light on protein aggregation as a mechanistic nexus in psychiatric disorders traditionally viewed through neurotransmitter imbalance paradigms alone. By targeting the protein misfolding cascade at its inception, the study pioneers a paradigm shift toward precision molecular psychiatry, where proteostatic vulnerabilities could be exploited to halt or reverse disease progression. Furthermore, this strategy may catalyze the discovery of analogous aggregation modulators for other neuropsychiatric conditions characterized by aberrant protein assemblies, such as bipolar disorder and major depressive disorder with psychotic features.
This study also addressed potential safety and off-target concerns inherent in protein aggregation inhibitors. Pharmacokinetic and toxicological profiling confirmed favorable tolerability, with no evidence of nonspecific protein destabilization or immune activation. The compound exhibited high blood-brain barrier permeability, sustained bioavailability, and predictable metabolic clearance, underscoring its suitability for translational development. Nevertheless, the authors caution that rigorous clinical trials are essential to validate efficacy and safety profiles in human populations, given interspecies differences in protein homeostasis and immune surveillance mechanisms.
Moreover, the researchers underscored the importance of incorporating advanced neuroimaging and biomarker identification into future studies to monitor therapeutic impact in real time and refine patient stratification criteria. For example, positron emission tomography (PET) ligands specific to DISC1 aggregates and functional magnetic resonance imaging (fMRI) indices of social brain network connectivity could serve as invaluable tools for optimizing dosing regimens and capturing response heterogeneity. The integration of molecular and systems neuroscience approaches will be pivotal in translating these preclinical successes into clinical breakthroughs.
At a mechanistic level, the study invigorates interest in dissecting the interplay between genetic risk factors and proteostatic dysfunctions in shaping the neurodevelopmental trajectory of schizophrenia. By illuminating how DISC1 aggregation disrupts synaptogenesis, dendritic spine morphology, and receptor trafficking, it enriches our understanding of the cellular architecture driving social cognition deficits. Concurrently, it highlights prospects for combining pharmacological proteostasis correction with behavioral interventions and neurostimulation therapies to achieve synergistic outcomes in restoring social functioning.
The research team’s collaborative and multidisciplinary effort epitomizes the power of converging technologies—ranging from structural biochemistry and in vivo behavioral neuroscience to computational biology—in pioneering therapies that could redefine psychiatric care. The ongoing refinement of DISC1-targeting molecules, bolstered by structure-activity relationship studies and medicinal chemistry innovation, heralds a new frontier in psychopharmacology where protein aggregation diseases, long confined to neurodegenerative disorders, gain central stage in psychiatric therapeutics.
As the global burden of schizophrenia and related disorders continues to escalate, driven largely by stigmatizing social impairments and functional disabilities, this advancement portends transformative clinical impact. Restoring social interaction not only ameliorates patient quality of life but also addresses cascading socioeconomic challenges associated with chronic psychiatric disability. This research beckons a future where molecularly targeted interventions can recalibrate disrupted neural networks, fostering recovery and reintegration for millions worldwide.
In sum, the identification and successful pharmacological targeting of DISC1 protein aggregation represent a watershed moment in schizophrenia research and beyond. By illuminating a hitherto underexplored etiological pathway and demonstrating its modifiability, this work propels the field toward precision neuropsychiatry, emphasizing molecular resilience as the cornerstone of therapeutic innovation. The forthcoming clinical translation of these findings holds promise not only for schizophrenia but also for a broad spectrum of neuropsychiatric disorders marked by synaptic and social dysfunction.
Subject of Research: Disrupted-in-Schizophrenia-1 (DISC1) protein aggregation and its role in social deficits in schizophrenia; pharmacological intervention to rescue social behavior in a rodent model.
Article Title: Pharmacological rescue of social deficits in rats featuring Disrupted-in-Schizophrenia-1 (DISC1) protein aggregation.
Article References: Dören, J., Van Gerresheim, E., Schäble, S. et al. Pharmacological rescue of social deficits in rats featuring Disrupted-in-Schizophrenia-1 (DISC1) protein aggregation. Schizophr (2026). https://doi.org/10.1038/s41537-026-00729-y
Image Credits: AI Generated