A groundbreaking new study led by researchers at McGill and Concordia universities has unveiled compelling evidence linking women’s subjective perceptions of their social status to early indicators of cardiac stress, potentially setting the stage for future heart disease. This research sheds light on a critical, yet understudied, dimension of cardiovascular risk—how social and psychological factors uniquely influence women’s heart health, underscoring the necessity for a paradigmatic shift in cardiac risk assessments and preventative strategies.
Cardiovascular disease remains the leading cause of death among women in North America, claiming one in every three female lives. Yet, paradoxically, women frequently receive less aggressive cardiac care than men, including fewer interventions and therapeutic treatments, often due to diagnostic tools and protocols primarily tailored around male physiology. Dr. Judy Luu, a clinician-scientist and Assistant Professor in McGill’s Department of Medicine, emphasizes that such disparities highlight a pressing need to reconsider not only medical but also psychosocial variables when evaluating cardiovascular risk specifically in women.
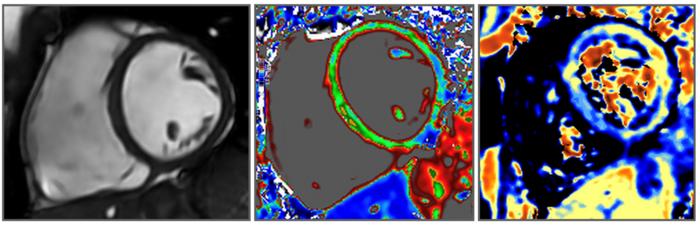
At the core of this study is the concept of subjective social status, which differs markedly from traditional socioeconomic metrics like income or educational attainment. Subjective social status captures an individual’s perceived rank within their social environment—how they feel about their own place in the societal hierarchy. Previous research has established associations between lower subjective social status and adverse physical and mental health outcomes, but this investigation is among the first to link these perceptions directly to measurable biological changes indicative of cardiac inflammation and fibrosis, using advanced cardiac magnetic resonance imaging (MRI).
Involving more than 400 adults aged between 35 and 83, all free of diagnosed heart disease, the study implemented a novel approach by asking participants to place themselves on a 10-rung ladder representing their social standing relative to others. Subsequent cardiac MRI scans assessed subtle but significant tissue changes—markers that often prelude overt cardiac dysfunction. Remarkably, women who rated themselves lower on the social ladder exhibited signs of inflammation and fibrotic scarring in their heart tissue, independent of objective socioeconomic parameters such as their income and education. Men with similar self-assessments did not show comparable cardiac alterations, indicating a sex-specific vulnerability.
The physiological mechanisms linking subjective social status to cardiac tissue changes remain an active area of inquiry. Jean-Philippe Gouin, co-lead author and Professor of Psychology at Concordia, posits two intersecting explanations. First, social self-perception may more accurately encapsulate women’s lived realities than traditional economic measures because women often face wage gaps, unequal caregiving responsibilities, and systemic social pressures, notwithstanding comparable educational achievements relative to men. Hence, these perceptions could serve as a more sensitive barometer of the psychosocial stressors influencing cardiovascular health.
Second, the psychological impact of perceiving oneself at a lower social status may induce chronic stress responses that potentiate cardiac inflammation. Chronic stress triggers a cascade of neuroendocrine and immune processes implicated in heart disease pathogenesis, including increased sympathetic nervous system activity and elevated levels of proinflammatory cytokines. Women reporting lower subjective social status may feel trapped by perceived limited opportunities for social mobility, exacerbating stress-induced biological damage.
These findings resonate with broader epidemiological data identifying stress as one of the top five risk factors for cardiovascular disease in women under 65—an age group where conventional risk factors such as hypertension or cholesterol imbalance may not fully explain disease onset. The observed cardiac MRI markers, indicative of inflammation and fibrosis, underscore the insidious nature of psychosocial stress impacts, potentially prefiguring more serious clinical manifestations if left unaddressed.
This research, while revealing, poses urgent clinical and public health questions: How can medical systems incorporate psychosocial assessments into routine cardiovascular care? How might these assessments influence the early identification and intervention strategies tailored for women at risk? Dr. Luu expresses hope that this work will catalyze a cultural shift, normalizing discussions about mental wellness, social contexts, and stress in cardiovascular risk evaluation and management.
Technologically, the use of cardiac MRI to detect subtle tissue-level changes offers an unprecedented window into preclinical disease states that previously eluded detection through standard diagnostic modalities. This imaging modality captures spatially resolved information on myocardial inflammation and fibrosis, thereby enabling researchers to observe biological footprints of stress and its gendered nuances with exceptional precision. Such insights provide a promising avenue for refining screening tools that move beyond traditional electrocardiograms or stress tests.
Future research directions include longitudinal follow-up with larger, diverse cohorts to establish the prognostic value of these early imaging markers in predicting clinical cardiovascular disease. Investigators also aim to disentangle complex biobehavioral pathways mediating the relationship between social perception, stress physiology, and cardiac health, potentially integrating biomarkers of inflammation with psychosocial questionnaires and neuroimaging.
The study invites cardiologists, psychologists, and public health experts alike to reframe their understanding of cardiovascular disease etiology, pushing beyond the conventional biomedical model to include sociocultural and psychological determinants. By acknowledging the sex-specific pathways through which societal positioning and lived experience modulate heart health, science takes a pivotal step towards precision medicine that truly accounts for gender dynamics.
In conclusion, this study spotlights a critical interface where subjective social standing and cardiovascular biology intersect uniquely in women, unveiling early cardiac tissue alterations tied to social perceptions of low status. It calls for heightened clinical awareness and a holistic approach incorporating mental and social health dimensions to forestall progression to symptomatic heart disease. As Dr. Luu articulates, shifting paradigms to embrace psychosocial risk factors in standard cardiac care protocol is not merely an academic exercise but an urgent imperative to save women’s lives.
Subject of Research: People
Article Title: Sex Differences in the Association Between Subjective Social Status and Imaging Markers of Cardiac Inflammation and Fibrosis
News Publication Date: 26-May-2025
Web References:
http://dx.doi.org/10.1097/PSY.0000000000001411
https://pubmed.ncbi.nlm.nih.gov/40471966/#:~:text=Compared%20to%20males%2C%20females%20demonstrated,sex%2Dspecific%20cardiovascular%20risk%20assessment.
References:
Biopsychosocial Science and Medicine, DOI: 10.1097/PSY.0000000000001411
Image Credits: Dr. Judy Luu
Keywords: Heart disease