In a breakthrough that could redefine the landscape of cancer therapeutics, researchers at the Center for Research in Biological Chemistry and Molecular Materials (CiQUS), University of Santiago de Compostela in Spain, have pioneered a novel molecular technique to enhance the intracellular delivery of anticancer drugs. Their focus is on doxorubicin, a cornerstone chemotherapy agent acclaimed for its efficacy but notorious for the emergence of drug-resistant cancer cells after prolonged treatment. This cutting-edge strategy hinges on the use of self-assembling cyclic peptide nanotubes which bypass conventional cellular resistance mechanisms, ensuring that doxorubicin reaches the nucleus where it exerts its lethal effect on tumor DNA.
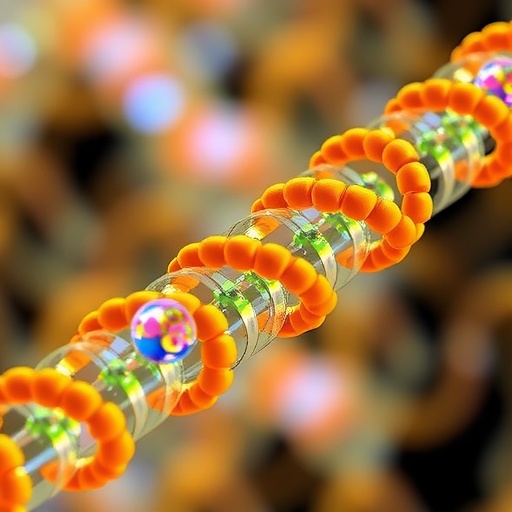
The crux of this innovative approach is the unique ability of cyclic peptides—small rings composed of amino acids—to spontaneously stack and organize into hollow cylindrical nanotubes. These nanostructures exhibit a profound affinity for cellular membranes rich in negatively charged lipids, a hallmark more prominent on the surface of cancer cells compared to their healthy counterparts. This physicochemical propensity empowers the peptides to selectively adhere to and penetrate malignant cells, effectively serving as Trojan horses delivering chemotherapeutic cargo directly inside the cellular fortress.
Importantly, the research team, led by chemist Juan R. Granja, chemically conjugated doxorubicin molecules to these cyclic peptides, engineering a sophisticated drug delivery system that defies the drug efflux pathways commonly responsible for doxorubicin resistance. Unlike the classical endocytic uptake where drugs are often sequestered or expelled, these nanotubes utilize an alternative internalization pathway, ensuring that resistance-prone cancer cells cannot effectively prevent nuclear drug accumulation. This re-routing of drug delivery potentiates doxorubicin’s cytotoxic capacity even in recalcitrant cancer phenotypes.
Mechanistically, the negatively charged lipid composition of cancer cell membranes acts as a beacon, attracting the cyclic peptide nanotubes whose surface contains positively charged residues and hydrophobic segments facilitating membrane insertion. As these peptide-drug conjugates self-assemble on the membrane surface, their nanotubular architecture promotes sustained interaction with the cell membrane that culminates in efficient permeation through the lipid bilayer. This intricate molecular dance is essential for the effective translocation of doxorubicin to the nucleus where it intercalates with DNA strands, inducing double-stranded breaks and subsequent apoptotic cell death.
Experimental data buttress the notion that the distinct chemical architecture of the cyclic peptides is pivotal for stable nanotube formation. Minor variations in amino acid sequence or ring size drastically influence the self-assembly process, thereby modulating cellular uptake and nuclear trafficking. These findings underscore the necessity for precise molecular design to optimize delivery efficiency and therapeutic index. The multidisciplinary team employed advanced spectroscopic and microscopic techniques, including atomic force microscopy and confocal imaging, to validate the morphology and intracellular distribution of the nanotube complexes.
This pioneering work was published in the prestigious journal ACS Applied Materials & Interfaces, affirming its scientific rigor and transformative potential. The study was undertaken at CiQUS, a recognized research center under the Xunta de Galicia, and is financially backed by the European Union via the Galicia FEDER Programme 2021–2027. This collaboration highlights the synergy between fundamental chemistry and translational cancer research, positioning peptide-based nanotechnology as an emerging frontier in oncological drug delivery.
One of the most formidable obstacles in current cancer therapy is multidrug resistance, where tumor cells activate membrane-bound pumps to expel chemotherapy agents, rendering treatments ineffective. By exploiting cyclic peptides as delivery vectors, this novel strategy circumvents these resistance pathways, facilitating intracellular doxorubicin accumulation in cells that would otherwise reject or metabolize the drug. This approach promises to rejuvenate the clinical utility of doxorubicin, extend patient survival, and potentially reduce side effects by lowering the requisite systemic dosage.
Combining the inherent selectivity for cancer cell membranes, robust nanoscale architecture, and controlled intracellular release mechanisms, these peptide nanotubes offer an elegant solution for delivering chemotherapeutics. Unlike conventional nanocarriers, the self-assembling nature of these cyclic peptides allows for modular optimization and functionalization, potentially accommodating a wide range of anticancer agents beyond doxorubicin. The flexibility of this platform could open new avenues for multiplexed drug delivery and combination therapies tailored to tumor-specific microenvironments.
Beyond drug delivery, cyclic peptide-based nanostructures may also serve as scaffolds for diagnostic tools and imaging agents, leveraging their biocompatibility and tunable surface chemistry. This integration of therapeutic and diagnostic modalities—so-called theranostics—could herald a personalized medicine era where treatment response can be monitored in real-time, ensuring timely clinical interventions and improved outcomes for patients battling resistant malignancies.
The implications of this discovery transcend the current chemotherapeutic paradigm. By rationally designing peptide sequences to exploit pathological lipid patterns on cancer cells, this research pioneers a new path for precision nanomedicine. The envisioned future involves iterative refinement of peptide chemistry to further enhance targeting specificity, cellular uptake kinetics, and payload release profiles, possibly extending applicability to other challenging cancers such as glioblastoma or metastatic breast tumors that are notoriously refractory to treatment.
Looking ahead, the research team envisions that incorporating this peptide nanotube technology into existing treatment regimens could substantially improve therapeutic indices and overcome barriers posed by tumor heterogeneity. Extensive preclinical trials and eventual clinical translation will be critical next steps to evaluate safety, dosage optimization, and potential immunogenicity. If successful, this approach could revolutionize chemotherapy, moving from a blunt force attack to a sophisticated targeted delivery system with heightened efficacy and minimized collateral damage.
In essence, this research epitomizes how innovative chemical engineering at the molecular level can redefine cancer therapy. Harnessing the natural proclivity of cyclic peptides to self-organize offers a promising strategy to surmount long-standing challenges of drug resistance. As cancer remains a leading cause of mortality worldwide, breakthroughs such as this bring renewed hope for more effective, tailored, and less toxic treatment modalities that ultimately save lives.
Subject of Research: Targeted delivery of anticancer drugs using cyclic peptide nanotubes to overcome drug resistance in cancer cells.
Article Title: Self-Assembling Cyclic Peptide Nanotubes for the Delivery of Doxorubicin into Drug-Resistant Cancer Cells
News Publication Date: 28-Aug-2025
Web References: DOI: 10.1021/acsami.5c05264
Image Credits: ACS Applied Materials & Interfaces 2025, 17, 36, 50191-50202. Copyright © 2025 The Authors. Published by American Chemical Society.
Keywords: Chemotherapy, Synthetic peptides, Peptide nanotubes, Drug resistance, Doxorubicin delivery, Nanomedicine, Cancer treatment, Cyclic peptides, Targeted drug delivery, Molecular self-assembly, Tumor cell membranes, Anticancer nanotechnology