In a stunning revelation emerging from the realm of pediatric medicine, researchers have identified a rare and insidious phenomenon involving occult medial orbital wall trapdoor fractures in children. This occurrence, although uncommon, can lead to severe complications, including recurrent rhinogenic intraorbital abscesses. The study led by Jiang et al., as reported in BMC Pediatrics, underscores a case that could reshape our understanding of orbital injuries in the pediatric population.
Orbital fractures, particularly those affecting the medial wall, are typically the result of blunt trauma. The mechanisms behind such injuries can vary, but in this case, the fracture remained concealed—hence the term “occult.” Unlike visible fractures, these injuries can slip under the radar, leading to dire consequences that may not manifest until much later. A pediatric patient presented with recurrent symptoms, prompting medical professionals to delve deeper into the possible underlying causes.
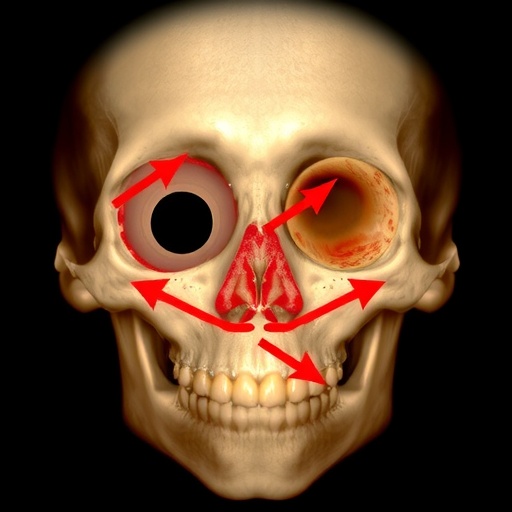
In children, the anatomy of the orbit is considerably different from that of adults. This anatomical disparity can complicate the diagnosis and management of orbital injuries. Children’s orbits are proportionally larger in relation to their cranial size, and the bones are less dense, which can lead to different types of injuries. Understanding these nuances is crucial for healthcare providers in diagnosing and managing such cases effectively.
This case report not only highlights the complexities associated with pediatric orbital fractures but also emphasizes the importance of a thorough examination. The initial symptoms may include nasal congestion and recurrent sinusitis, which can easily mislead practitioners to overlook potential underlying issues in the orbit. As such, a high index of suspicion is needed, particularly in young patients who present with seemingly non-specific or vague symptoms.
The implications of ignoring an occult fracture can lead to recurrent abscess formation within the orbit, a complication seen in the reported case. Facing a recurrent rhinogenic intraorbital abscess presents both diagnostic and therapeutic challenges. Typically, managing such an abscess would involve antibiotics and, in certain cases, surgical intervention, highlighting the multifaceted nature of treatment that may be warranted for pediatric orbital injuries.
In the study, the authors presented the clinical journey of a young patient who suffered from these complications. The meticulous documentation of symptoms, diagnosis, and treatment provided valuable insights for healthcare workers dealing with similar cases. Their findings underscore the need for an integrated approach, combining surveillance, imaging, and possibly surgical intervention, to improve outcomes for pediatric patients with orbital injuries.
Imaging plays a pivotal role in diagnosing occult fractures. A CT scan is often the gold standard, allowing for high-resolution axial and coronal views of the orbits. The identification of subtle fractures, especially those hidden from direct view, is crucial in determining an appropriate treatment plan. In this case, advanced imaging techniques helped delineate the fracture and inform surgical decision-making, emphasizing the necessity of using advanced diagnostics in atypical presentations.
Pediatric patients often exhibit different responses to surgical interventions compared to adults. Their healing processes, anatomical changes as they grow, and the psychological dimensions of surgery can all differ markedly. As such, the implementation of a treatment plan must be tailored to the pediatric demographic, which can sometimes complicate direct comparisons with adult cases.
There is also a significant gap in awareness regarding these types of injuries among general practitioners. Enhancing education and training can facilitate better recognition and management of occult fractures in children. With proper awareness, there is a potential to reduce the incidence of long-term complications associated with undiagnosed orbital injuries.
Furthermore, this report raises questions about the long-term follow-up for pediatric patients with such injuries. As children grow, regular monitoring becomes essential to ensure proper healing and to watch for any late-onset complications. The establishment of dedicated follow-up protocols could significantly improve quality of care.
In summary, Jiang et al.’s report serves as an important reminder of the intricate nature of pediatric orbital fractures. The ramifications of overlooking subtle signs can lead to severe complications that compromise not only ocular health but general well-being. Ultimately, continuous education, thorough examination, and advanced diagnostic imaging are essential in tackling these complex cases effectively.
The narrative of this young patient’s journey from misdiagnosis to eventual proper intervention is a call to action for healthcare systems. It emphasizes both the need for vigilance in cases that appear innocuous and the importance of interdisciplinary collaboration in managing complex pediatric cases. As awareness grows, there is hope for improved diagnostic protocols and treatment avenues that will safeguard the health of future generations.
In summary, the prevention, recognition, and treatment of occult medial orbital wall fractures requires a collective effort from researchers, medical professionals, and educators. By fostering a comprehensive understanding of these rare yet significant injuries, pediatric healthcare can embrace a future that prioritizes detection and timely intervention, ultimately enhancing the quality of care for young patients facing such challenges.
Subject of Research: Occult medial orbital wall trapdoor fractures in pediatric patients and their complications.
Article Title: Occult medial orbital wall trapdoor fracture inducing recurrent rhinogenic intraorbital abscess in a pediatric patient: a case report.
Article References:
Jiang, L., Jiang, X., Wu, W. et al. Occult medial orbital wall trapdoor fracture inducing recurrent rhinogenic intraorbital abscess in a pediatric patient: a case report.
BMC Pediatr 25, 942 (2025). https://doi.org/10.1186/s12887-025-06331-y
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12887-025-06331-y
Keywords: pediatric orbital fractures, occult fractures, medial wall, rhinogenic abscess, CT imaging, pediatric healthcare, intraorbital abscess.