In recent years, the phenomenon of migrant mortality advantage has captured the attention of demographers and public health experts across the globe. This intriguing observation—that migrants often exhibit lower mortality rates than native-born populations—poses essential questions about the interplay between migration, health, and longevity. A groundbreaking new study, led by Flici, Trias-Llimos, and Permanyer, explores this phenomenon within the context of Spain, shedding new light on how migrants’ origins significantly shape their mortality profiles. The findings propel a nuanced understanding of how origin affects mortality advantages among migrant populations, offering unprecedented insights into the public health landscape of modern Spain.
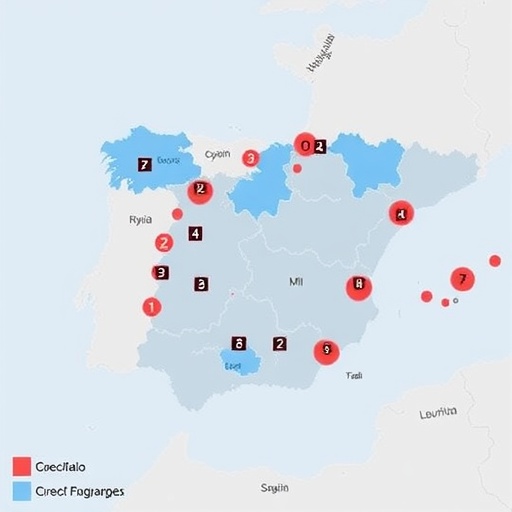
The study investigates mortality patterns across various migrant groups residing in Spain, analyzing a wealth of demographic and epidemiological data. Prior research has established that migrants often demonstrate a mortality advantage—a somewhat paradoxical trend given the myriad challenges they face, including socioeconomic hardships, integration issues, and access to healthcare. However, this research uniquely dissects how the mortality advantage varies depending on migrants’ country or region of origin. Such differentiation is paramount because it acknowledges the heterogeneity among migrant populations, challenging the tendency to treat migrants as a monolithic group in epidemiological studies.
By leveraging extensive administrative records and mortality data, the researchers conducted a comparative analysis that highlights distinct mortality trajectories between different migrant origin groups. For instance, migrants from certain Latin American countries displayed notably lower mortality rates in comparison to both the native Spanish population and other migrant cohorts. This disparity underscores the critical role that cultural, socioeconomic, and pre-migration health conditions play in shaping migrants’ health outcomes post-arrival. The implications are profound, suggesting that country of origin influences not only initial health status but also ongoing health trajectories within the host country.
A key aspect of the study is its methodological rigor. Utilizing age-standardized mortality rates enables the researchers to account for the differing age structures of migrant groups, ensuring that comparisons with the native population remain valid and statistically robust. Additionally, the study controls for a range of sociodemographic variables, including socioeconomic status and duration of residence in Spain, to isolate the pure effect of origin on mortality advantage. This multifaceted approach strengthens the validity of the findings, providing a comprehensive portrait of the health dynamics within Spain’s diverse migrant populace.
Intriguingly, the research also explores how mortality advantages evolve with increasing duration of stay in Spain. Longitudinal analyses reveal that the initial mortality advantage observed in many migrant groups tends to attenuate over time, a pattern that appears to be influenced by a process often referred to as the ‘acculturation paradox.’ This phenomenon theorizes that while initial arrivals may exhibit superior health profiles, the adoption of host country behaviors and lifestyles can erode this advantage. The study’s findings on this front are particularly illuminating, highlighting how the endurance and magnitude of mortality advantage differ significantly among various origin groups, thus emphasizing the complexity inherent in the migrant health experience.
Further, the authors engage with theoretical frameworks explaining why migrants tend to experience lower mortality, notably the “healthy migrant effect” and the “salmon bias.” The healthy migrant effect posits that migrants are a self-selected group of healthier individuals who choose to migrate, thus skewing mortality profiles positively. Meanwhile, the salmon bias hypothesis suggests that some migrants return to their home countries when seriously ill or near death, artificially lowering mortality rates observed in the host country data. The study examines these theories within the Spanish context, offering reflections based on empirical data that reveal the extent to which these effects manifest across origin groups.
The findings also have profound implications for public policy and health programming. Understanding that the mortality advantage is not uniform but modulated by origin underscores the need for tailored health interventions that recognize the specific vulnerabilities and strengths of different migrant communities. Such insights could refine Spain’s healthcare strategies to more effectively address the unique health landscapes of migrant groups, ensuring equitable access to care and the promotion of healthy aging across diverse populations.
From a broader scholarly perspective, the research enriches the ongoing discourse about the social determinants of health, emphasizing migration as a critical variable in the epidemiological equation. It challenges simplistic narratives around migrant health, advocating for a more intersectional analysis that integrates factors like origin, socioeconomic position, and cultural practices into mortality research. By doing so, it sets a new benchmark for future studies seeking to unravel the complex tapestry of migration and health outcomes in an increasingly globalized world.
The implications of this study resonate beyond Spain’s borders, providing a framework that might be applicable to other European countries experiencing diverse migration flows. The heterogeneity observed among migrant origin groups in Spain mirrors trends witnessed in other nations, suggesting that policies and health strategies developed in one context could inspire analogous initiatives elsewhere. This transnational relevance amplifies the study’s significance, positioning it as a vital contribution to international migration and health scholarship.
Moreover, the research highlights the necessity of granular data collection and analysis to capture the intricate health patterns by migrant subgroups. The study advocates for improved data infrastructure and integrated health surveillance that can disaggregate migrants according to origin and other critical variables. Such data precision is essential not only for academic inquiry but also for pragmatic public health planning and resource allocation.
In the context of aging populations across Europe, the study’s insights gain further urgency. Migrant populations often represent a younger demographic, yet understanding their mortality trajectories informs projections for future demographic shifts and healthcare needs. This information is particularly useful for anticipating the pressures on social security systems and long-term care facilities, underscoring the intersection between migration, mortality, and economic sustainability.
Additionally, the research confronts stereotypes and misconceptions about migrant health. By revealing that the mortality advantage is not monolithic but varies by origin, it challenges simplistic assumptions that migrants as a whole are either uniformly healthier or disadvantaged. This nuanced portrayal fosters a more informed and empathetic public discourse surrounding migration, health equity, and social integration.
The study also prompts reflections on the interplay between migration policies and health outcomes. For instance, how policies related to access to health services, legal status, and social inclusion might mediate the observed mortality patterns remains a fertile area for further investigation. The Spanish context provides a valuable case study to explore these policy-health intersections, with potential lessons for other countries navigating complex migration landscapes.
In synthesizing their complex findings, the authors call for ongoing research to deepen the understanding of the mechanisms behind the mortality advantage and its variation by origin. They emphasize the importance of interdisciplinary approaches that integrate demographic methods, epidemiology, sociology, and public health. Such comprehensive inquiry is pivotal to fully unveil the dynamics shaping migrant mortality and to design effective, equitable interventions.
Ultimately, this study marks a significant leap forward in our comprehension of migrant health, particularly in illuminating how origin critically influences mortality advantages. It moves beyond broad generalizations, offering a finely tuned analysis that enriches both academic knowledge and practical policy frameworks. As demographic shifts continue to reshape Europe, insights such as these will prove essential in crafting societies that promote health and well-being for all, irrespective of origin.
Subject of Research: The influence of country or region of origin on the migrant mortality advantage in Spain.
Article Title: How does origin affect migrant mortality advantage in Spain?
Article References:
Flici, F., Trias-Llimos, S. & Permanyer, I. How does origin affect migrant mortality advantage in Spain?. Genus 81, 22 (2025). https://doi.org/10.1186/s41118-025-00264-1
Image Credits: AI Generated