In a groundbreaking pilot study published in 2025, researchers have made significant strides in the field of forensic neuroimaging by optimizing inversion time parameters in postmortem brain imaging using 1.5 Tesla Fluid-Attenuated Inversion Recovery (FLAIR) MRI technology. This advancement offers promising new avenues for the detailed investigation of neuropathological changes after death, potentially transforming both forensic medicine and neuropathology.
Magnetic resonance imaging (MRI) has long been a tool of choice for visualizing the brain’s complex anatomy and pathology. However, postmortem imaging presents unique challenges that require specialized technique adjustments. Key among these is the selection of the inversion time (TI) in FLAIR sequences. TI is crucial because it affects the suppression of cerebrospinal fluid (CSF) signals, thereby influencing the contrast and visibility of brain lesions or abnormalities. Fine-tuning this parameter for postmortem conditions, as opposed to in vivo imaging, could greatly enhance diagnostic accuracy.
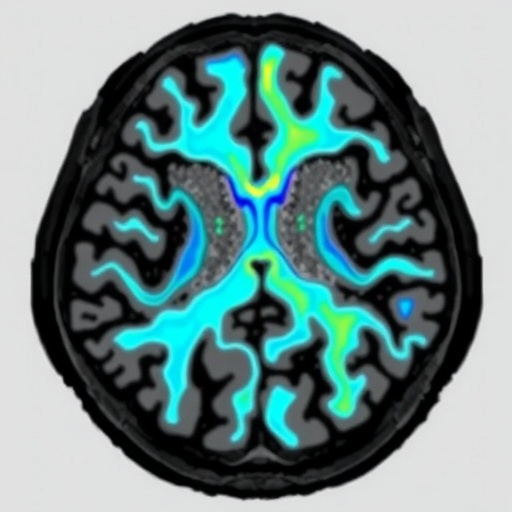
The study utilizes a 1.5 Tesla MRI scanner equipped with FLAIR pulse sequences, examining a range of inversion times for optimal image quality in cadaveric brain tissue. Given the physiological changes after death—such as alterations in tissue relaxation times and fluid properties—the standard inversion times used in clinical contexts may not be suitable. Adjusting TI accordingly allows for clearer delineation of pathological features such as edema, hemorrhage, or infarcts, all of which are critical for forensic diagnoses.
One of the central innovations of this research lies in its meticulous approach to postmortem tissue characterization. The investigators tested a spectrum of inversion times, systematically assessing image contrast, signal-to-noise ratio, and the extent of CSF suppression. They discovered that conventional TI values require significant modification to achieve optimal results, highlighting the fundamental difference between living and deceased brain environments in the MRI context.
This methodological refinement carries enormous forensic value. In forensic neuropathology, distinguishing subtle pathologies can inform the determination of cause and time of death, contributing essential evidence to medico-legal investigations. Enhanced MRI imaging fidelity aids in identifying markers of trauma, hypoxic injury, or neurodegenerative changes, which may be imperceptible during standard autopsy or unoptimized imaging.
Beyond forensic applications, this optimized imaging technique may have implications for neuropathological research. Postmortem MRI can bridge the gap between clinical neuroimaging and histological studies by providing in situ, non-destructive views of brain pathology. The clarity afforded by the optimized FLAIR parameters facilitates more accurate correlation between imaging findings and microscopic tissue analysis.
Technically, the study addresses the complex physics of MRI signal generation and decay under postmortem conditions. Tissue relaxation times, particularly T1 and T2, change after death due to factors such as temperature variation, cessation of metabolic processes, and tissue decomposition. These changes disrupt the delicate balance required for CSF suppression in FLAIR sequences, which the adjusted TI values compensate for effectively.
The researchers also accounted for variabilities introduced by postmortem interval—the time elapsed since death—which can affect tissue hydration and MR properties. Their protocol suggests that inversion time optimization must be flexible and tailored according to these intervals, further underscoring the need for customized imaging protocols in forensic contexts.
Crucially, the study’s results were validated by comparing MRI findings with histopathological examination, ensuring that the optimized inversion time indeed enhanced the visibility of relevant pathological features. This cross-validation grounds their imaging protocol in biological reality, providing confidence in its practical applicability.
Another notable aspect of this work involves its potential to standardize postmortem brain imaging protocols. Presently, a lack of consensus on imaging parameters contributes to heterogeneous results and inconsistent interpretation, hampering broader forensic or clinical integration. This pilot study’s data-driven recommendations could lead to the establishment of benchmarking standards for postmortem MRI.
The implications extend to the medico-legal domain, where digital imaging evidence is critically scrutinized. High-quality MRI scans with optimized inversion times may supplement traditional autopsies, helping to confirm or challenge initial findings, provide corroborative evidence, or even detect pathologies that would otherwise remain undetected.
With increasing interest in minimally invasive autopsy techniques, this optimization of FLAIR MRI parameters aligns perfectly with the emerging trend toward integrating imaging into forensic workflows. It offers an efficient, non-destructive adjunct tool that respects cultural sensitivities limiting conventional autopsy and improves the investigation process.
From a technical perspective, the study highlights the importance of FLAIR sequences in postmortem imaging. FLAIR’s ability to suppress CSF signals is invaluable to highlighting brain tissue abnormalities, but postmortem changes require a reconsideration of inversion times. The findings shed light on how to recalibrate these parameters for enhanced contrast and detail.
Furthermore, the research underscores the need for tailored MRI protocols based on magnet strength—in this case, 1.5 Tesla—as results might differ on higher field strengths like 3T or 7T scanners. The researchers emphasize careful protocol adaptation depending on available hardware and specific forensic needs.
The production of high-fidelity postmortem brain images facilitates more precise research into neurodegenerative diseases and brain injuries by allowing detailed visualization without tissue extraction. This capability opens up possibilities for longitudinal studies linking clinical symptoms, imaging, and postmortem results.
In conclusion, this pioneering study by Bruguier, Magnin, Knebel, and colleagues represents a pivotal advancement in forensic neuroradiology. Their careful optimization of inversion time in 1.5 Tesla postmortem FLAIR MRI demonstrates how adjusting technical parameters to postmortem tissue dynamics can drastically improve diagnostic yields. This progress not only enhances medico-legal investigations but also sets the stage for future innovations in postmortem imaging research and practice.
As forensic medicine continues to embrace technological integration, such innovations promise to refine death investigations, improve accuracy, and ultimately, serve justice more effectively. The optimized postmortem MRI protocols may soon become a standard part of neuropathological examinations worldwide, marking a new era where imaging advances profoundly impact forensic sciences.
Subject of Research: Postmortem brain imaging and inversion time optimization in 1.5 Tesla FLAIR MRI
Article Title: Inversion time optimization in postmortem 1.5 tesla FLAIR brain imaging: a pilot study
Article References:
Bruguier, C., Magnin, V., Knebel, JF. et al. Inversion time optimization in postmortem 1.5 tesla FLAIR brain imaging: a pilot study. Int J Legal Med (2025). https://doi.org/10.1007/s00414-025-03571-6