In recent years, the ongoing COVID-19 pandemic has accentuated the importance of understanding viral mutations and their implications for human health. SARS-CoV-2, the virus responsible for COVID-19, has undergone multiple mutations since its emergence, leading to various variants that exhibit differing characteristics. Among these, the Omicron variant has become particularly noteworthy due to its rapid spread and enhanced transmissibility. Researchers, including Chang et al., have delved into the specific binding affinities of peptides derived from the Omicron variant, focusing on their interactions with population-specific Human Leukocyte Antigens (HLAs).
Human HLAs are critical components of the immune system. They play a pivotal role in the recognition of viral peptides by T cells, which are essential for mounting an effective immune response. The binding affinity of these viral peptides to HLAs can significantly influence the immune response generated by an individual’s body, ultimately affecting the degree of protection against the virus. Variations in HLA compositions across different ethnic groups can further complicate this relationship, leading to disparities in immunity and disease outcomes.
In their recent study published in the Journal of Biomedical Science, Chang and colleagues have made groundbreaking strides in characterizing the changes in binding affinity associated with the peptides of the SARS-CoV-2 Omicron variant. By employing sophisticated biochemical techniques and computational modeling, the researchers aimed to elucidate how these changes could potentially impact the immune response in diverse populations. The study highlights the critical need to understand the nuances of viral evolution, especially considering the implications for vaccine development and therapeutic strategies.
One prominent focus of the research was the methodology utilized to assess the binding affinities of the peptides. The researchers employed a technique known as peptides-MHC binding assays, a powerful tool used to quantify how effectively viral peptides associate with HLAs. This methodology is not only pivotal for comprehension of potential immune responses but also allows for comparisons between different variants of the virus.
As the study progressed, it became evident that the Omicron variant peptides demonstrated altered binding affinities compared to those derived from previous variants. This change raised concerns about the efficacy of existing vaccines, as these vaccines are primarily designed based on the original strain of the virus. When the immune system has altered targets to recognize, the effectiveness of neutralization can also be compromised, leading to an increased likelihood of breakthrough infections and reinfections among vaccinated individuals.
The researchers also noted the significance of population-specific HLA types. Different ethnic groups possess unique distributions of HLA alleles, which can affect how well the immune system responds to various viral peptides. For instance, some populations may have HLAs that bind more effectively to Omicron peptides, potentially providing them with enhanced protection. Conversely, other populations may have a less robust response, highlighting the necessity for tailored vaccine strategies that consider these genetic variations.
Biologically, the interaction between HLAs and viral peptides is a complex process. The conformation of the peptide and its ability to fit into the binding groove of the HLA molecule are essential factors determining binding strength. Furthermore, subtle changes in the amino acid composition of the peptides can either enhance or reduce their affinity for specific HLAs. The findings from Chang et al. elucidate how such fine-tuned interactions among variants can significantly influence pandemic dynamics and underlie differing health outcomes in populations.
The study also sheds light on the broader implications of viral evolution. As the SARS-CoV-2 virus continues to mutate, understanding the binding affinities of emerging variants is crucial for predicting future trends in transmissibility and the effectiveness of public health interventions. This research contributes to a growing body of evidence supporting the need for constant surveillance of viral strains and adaptation of vaccine formulations to align with evolving variants.
Another important aspect covered in the investigation is the concept of immune evasion. The Omicron variant has exhibited an ability to evade immune detection better than its predecessors. This is partly due to mutations in the spike protein, which is the target for most vaccines. The ability of this variant to bind poorly or differently to certain HLAs means that even vaccinated individuals may not mount an adequate immune response, leading to an increase in cases.
The implications of such findings cannot be overstated. If specific populations are found to have lower binding affinities for Omicron peptides, public health officials may need to rethink strategies for vaccine distribution and deployment. Personalized medicine could become a reality in vaccine administration, with the potential to tailor vaccines to enhance efficacy within diverse communities based on their individual HLA profiles.
Understanding the binding affinity changes associated with different variants presents vital knowledge for the future of vaccine research and development. The landscape of virology is constantly evolving, and ongoing studies like that of Chang et al. emphasize the need to adapt to these changes proactively. The dynamics of the immune system and viral interaction are intricate, yet they hold the key to overcoming future challenges presented by emerging variants of concern.
As we continue to navigate the complexities of the COVID-19 pandemic, insights from studies regarding binding affinities serve as a crucial reminder of the underlying mechanisms that dictate infectious disease dynamics. Researchers and healthcare professionals must remain vigilant, continuously updating their knowledge to ensure that public health responses are informed and effective.
Moreover, the scientific community’s collaborative efforts in the face of this global health crisis have paved the way for rapid advancements in our understanding of SARS-CoV-2 and its variants. Studies like the one conducted by Chang and colleagues contribute vital information that can guide policymaking, vaccine design, and the preparation for potential future pandemics.
In conclusion, understanding the changes in binding affinity of SARS-CoV-2 Omicron variant peptides to population-specific HLA is a critical area of research. As we learn more about these interactions, we improve our chances of effectively combating the virus and adapting our public health strategies. The implications of this research extend beyond the current pandemic, providing insights into the future of viral infections and the biotechnology industry.
Subject of Research: Changes in binding affinity of SARS-CoV-2 Omicron variant peptides to population-specific HLAs.
Article Title: Characterization of binding affinity changes of SARS-CoV-2 omicron variant peptides to population-specific HLA.
Article References:
Chang, CM., Wu, CJ., Shkurnikov, M. et al. Characterization of binding affinity changes of SARS-CoV-2 omicron variant peptides to population-specific HLA.
J Biomed Sci 32, 44 (2025). https://doi.org/10.1186/s12929-025-01139-5
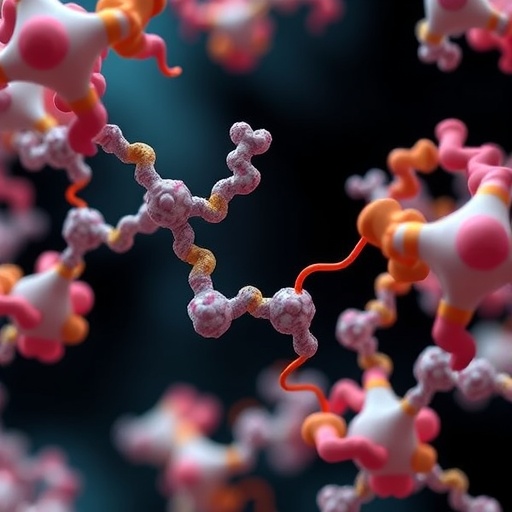
Image Credits: AI Generated
DOI: 10.1186/s12929-025-01139-5
Keywords: SARS-CoV-2, Omicron variant, binding affinity, Human Leukocyte Antigen, immune response, viral mutations, population genetics, vaccine strategy, public health.