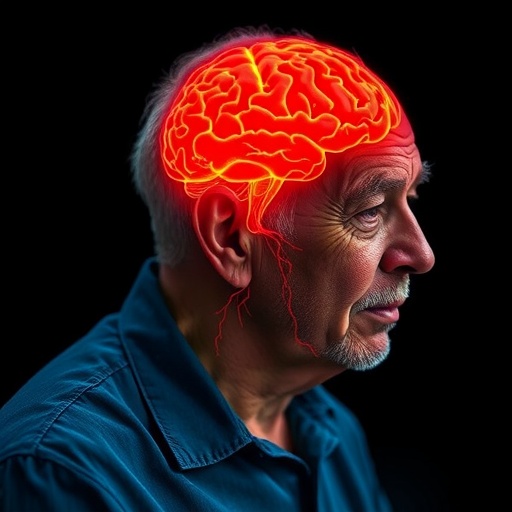
Emerging research illuminates a compelling nexus between traumatic brain injuries (TBI) sustained in late adulthood and an elevated incidence of dementia, alongside increased care demands. This comprehensive population-based cohort study, published in the Canadian Medical Association Journal, charts novel territory in understanding the long-term neurological and social consequences of TBI among older adults aged 65 and above.
Traumatic brain injuries, characterized by direct or indirect mechanical forces to the skull and brain—for example, from falls or abrupt acceleration-deceleration injuries like whiplash—lead to a constellation of acute neurological impairments. These include loss of consciousness, amnesia, disorientation, and focal neurological deficits such as impaired motor coordination or speech disturbances. While TBIs affect all age groups, their incidence and impact in the elderly are particularly pronounced due to physiological vulnerabilities and frequently occur as a result of falls, which account for over half of TBI cases in this demographic.
The study rigorously analyzed data from over 260,000 senior adults across a 16-year span beginning in 2004, meticulously comparing those with newly diagnosed TBIs against those without brain injury. The investigators followed participants longitudinally for the development of dementia, mortality, and patterns of care utilization. Their observations revealed that a new TBI diagnosis in later life corresponded with a dramatically increased risk of dementia onset—approximately a 69% higher hazard ratio within the first five years post-injury and sustaining at a 56% increased risk beyond that five-year mark. This enduring association underscores the profound neuropathological consequences of brain trauma even when sustained in advanced age.
Beyond dementia risk, the study highlighted augmented needs for publicly funded home care services among TBI survivors, who averaged 87 days of care annually compared to 84 days for their counterparts without brain injury. This subtle yet statistically significant increase in care dependency reflects the broader functional decline linked to TBI sequelae, encompassing cognitive, motor, and psychosocial domains. Moreover, certain sociodemographic factors modulated these outcomes; increasing age and female sex emerged as significant modifiers of dementia risk post-TBI, with women and those aged 85 and older exhibiting particularly elevated vulnerability.
Socioeconomic disparities further compounded risk stratification. Older adults dwelling in low-income neighborhoods faced disproportionately higher dementia rates following TBI, illuminating the intersection of social determinants of health and neurotraumatic outcomes. This observation was paralleled by increased long-term care admissions among individuals in smaller rural or less ethnically diverse communities—populations that often grapple with constrained healthcare resources and accessibility challenges. These disparities signal urgent need for targeted public health strategies that integrate socioeconomic context in mitigating post-TBI dementia risk and care burdens.
The findings bear critical implications for healthcare delivery and policy. They advocate for prioritizing specialized community-based dementia prevention programs and support infrastructure tailored to high-risk subpopulations, notably women over 75 residing in economically disadvantaged or rural settings. Such interventions could disrupt the trajectory toward institutionalization and enhance quality of life through early rehabilitation, cognitive stimulation, and fall-prevention initiatives.
From a mechanistic standpoint, the persistent increase in dementia risk following late-life TBI invites deeper exploration into injury-induced neurodegenerative processes. Traumatic insults may trigger cascades of chronic neuroinflammation, axonal injury, and proteinopathies resembling Alzheimer’s disease pathology. Moreover, brain reserve diminishes with age, potentially exacerbating susceptibility to cumulative insult. These biological underpinnings align with epidemiological data, reinforcing the urgency of mitigating fall-related TBI occurrences.
Clinicians are thus equipped with critical prognostic insights from this research, enabling more informed counseling of older patients and families regarding the potential long-term neurological consequences of TBI. Integrating tailored surveillance for cognitive decline post-injury can facilitate timely interventions and planning for augmented care needs. Additionally, these data reinforce the imperative of fall-prevention strategies—ranging from home safety modifications to balance and strength training programs—to attenuate the initial injury risk.
This study, grounded in observational methodology and leveraging extensive population cohorts, advances understanding of the multifaceted outcome landscape following TBI in aging populations. It not only delineates the quantitative escalations in dementia risk and care dependency but weaves in granular sociocultural dimensions that shape health trajectories. The knowledge serves as a clarion call for multidisciplinary approaches uniting neurology, geriatrics, public health, and social services to holistically address this growing healthcare challenge.
Future research directions entail elucidating biomarkers predictive of dementia progression post-TBI and intervention trials to mitigate neurodegeneration. Leveraging longitudinal imaging, fluid biomarkers, and genetic profiling could unravel patient-level risk stratification. Furthermore, innovative care models that blend medical treatment with social support may enhance outcomes and reduce healthcare system burdens.
In summary, this landmark cohort investigation underscores that traumatic brain injury in late life is not a transient event but a pivotal risk factor precipitating cognitive decline and augmented care needs. As the global population ages, concerted efforts in prevention, early detection, and targeted support are paramount to curbing the societal and individual impact of TBI-related dementia. The research paves the path for nuanced clinical guidance and health policy reforms aimed at safeguarding cognitive health in elderly populations vulnerable to brain trauma.
Subject of Research: People
Article Title: Rate of incident dementia and care needs among older adults with new traumatic brain injury: a population-based cohort study
News Publication Date: 6-Oct-2025
Web References: https://www.cmaj.ca/lookup/doi/10.1503/cmaj.250361
References: 10.1503/cmaj.250361
Keywords: Dementia, Brain injuries, Gerontology, Aging populations, Geriatrics, Older adults