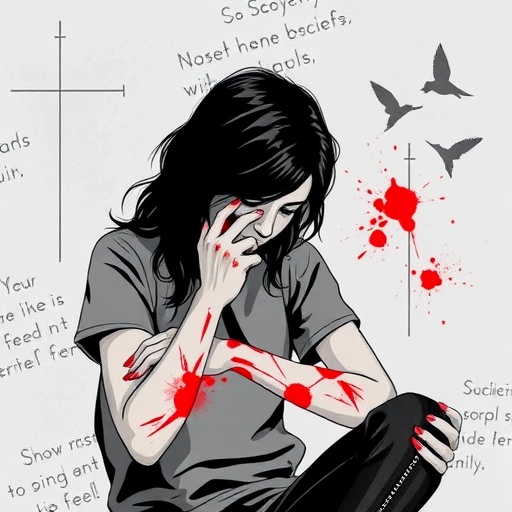
In recent years, non-suicidal self-injury (NSSI) has emerged as a significant public health concern, particularly among adolescents diagnosed with depressive disorders. A groundbreaking review published in BMC Psychiatry delves into the multifactorial elements influencing NSSI behaviors, shedding light on the complex interplay of psychological, behavioral, and environmental factors that drive these self-harm actions. This comprehensive analysis provides critical insights that could help reshape preventive and intervention strategies for this vulnerable population.
NSSI encompasses deliberate harm to one’s own body without suicidal intent, often manifesting as cutting, burning, or scratching. These behaviors, while non-lethal, carry serious implications for adolescents’ mental health, escalating risks for future suicidal actions and long-term psychological distress. The review in question synthesizes findings from 15 rigorous studies, including systematic reviews, cross-sectional analyses, and clinical guidelines, offering a panoramic view of the current understanding surrounding adolescent NSSI within the context of depression.
Crucially, the research underscores the necessity of viewing NSSI not merely as a symptom of depressive disorders but as a distinct behavioral phenomenon influenced by a multitude of factors. These include individual characteristics such as age, gender, and sexual orientation, which can predispose certain adolescents to engage in self-injury. The nuanced role of psychological traits—ranging from impulsivity to emotional regulation difficulties—further complicates these behaviors, suggesting that psychological assessments must extend beyond core depressive symptoms.
Beyond individual traits, illness- and treatment-related aspects also critically inform NSSI risk. The duration and severity of depression emerged as significant correlates, reflecting how protracted or intense depressive episodes can exacerbate self-injurious tendencies. This link emphasizes the importance of timely and effective management of depressive symptoms to potentially curb the onset or escalation of NSSI. Moreover, the study acknowledges the treatment landscape’s complexities, hinting at the need for integrative therapeutic approaches tailored to the adolescent’s unique condition.
Lifestyle factors notably contribute another layer of risk modulation. The review highlights associations between behavioral patterns such as internet addiction and exposure to stressful life events with heightened NSSI prevalence. These observations call for holistic intervention models that incorporate lifestyle and behavioral counseling alongside traditional psychiatric care, recognizing the digital environment as a modern-day influencer of mental health behaviors.
Family dynamics and social environments stand out as critical contextual variables. Dysfunctional family functioning and insufficient social support were consistently linked with increased NSSI behaviors, pointing to the foundational role of the adolescent’s immediate social milieu. This insight stresses that preventive measures cannot afford to ignore the broader relational context, advocating for family-inclusive therapeutic frameworks and strengthened community support systems.
Importantly, the review pioneers a risk-grading-based preventive intervention framework aimed at stratifying adolescents according to their NSSI risk profile by integrating these diverse factors. Such a framework would allow clinicians to tailor interventions more precisely, allocating resources efficiently and enhancing therapeutic outcomes. The incorporation of a multidimensional assessment tool into clinical practice represents a significant advance toward personalized mental health care for depressed adolescents.
The authors of the review call attention to the current gaps in predictive modeling of NSSI risk. Validating identified risk factors through prospective studies and testing intervention measures’ efficacy remain imperative future directions. This focus on empirical validation underscores the ongoing evolution of understanding in this domain, aiming to transition from correlation-driven insights to causality-informed clinical applications.
At a broader scale, these findings resonate with global mental health priorities, emphasizing adolescent mental wellness as a pivotal preventive frontier. The escalating rates of NSSI in depressed youth symbolize not only individual suffering but also systemic gaps in mental health infrastructure and education. By disseminating this knowledge, the review catalyzes awareness within the psychiatric community and beyond, encouraging multipronged strategies to mitigate NSSI’s burden.
Technically, the review employed Arksey and O’Malley’s scoping review methodology—a systematic yet flexible approach suited for exploring broad and complex topics. This method facilitated the aggregation and analysis of heterogeneous evidence, ensuring a comprehensive synthesis that encompasses clinical guidelines, empirical studies, and literature reviews. Such rigorous methodological anchoring enhances the credibility and applicability of the review’s conclusions.
In clinical practice, the translational impact of these insights is profound. Psychiatrists, psychologists, and pediatricians are urged to integrate multifaceted risk factor assessments into routine evaluations of depressed adolescents. The traditional focus on symptomatic treatment alone must expand to encompass psychological traits, social factors, and lifestyle patterns. This holistic lens promises to identify at-risk individuals earlier and foster more nuanced, effective interventions.
As the field advances, digital health innovations and data analytics may offer new pathways to operationalize these findings. For instance, machine learning algorithms could synthesize patient data across domains to generate real-time risk profiles, enabling dynamic, personalized care plans. Simultaneously, interactive family and social support platforms might mitigate environmental risk factors, representing a novel axis for intervention.
Ultimately, this pioneering review serves as a clarion call for multidisciplinary collaboration, integrating psychiatry, psychology, social work, and digital health to confront the intricate challenge of NSSI in adolescents with depression. The hope is that through informed, multi-layered strategies, the frequency of self-injury behaviors can be reduced, and the trajectory toward suicidality can be interrupted, safeguarding the mental health and future well-being of young individuals worldwide.
Subject of Research: Non-suicidal self-injury behavior in adolescents with depressive disorders and related influencing factors
Article Title: A review of the scope of non-suicidal self-injury behavior in adolescents with depressive disorders: an analysis of related influencing factors
Article References: Ling, Y., Gu, Y., Solomon, O.M. et al. A review of the scope of non-suicidal self-injury behavior in adolescents with depressive disorders: an analysis of related influencing factors. BMC Psychiatry 25, 913 (2025). https://doi.org/10.1186/s12888-025-07361-7
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12888-025-07361-7
Keywords: Non-suicidal self-injury, adolescent depression, risk factors, psychological traits, family environment, depression severity, behavioral patterns, preventive intervention