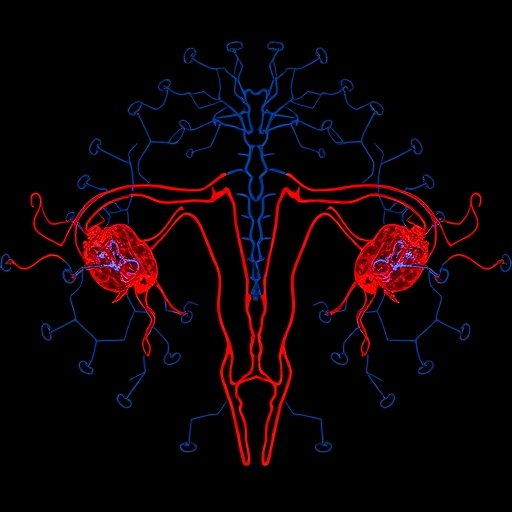
In a groundbreaking development poised to reshape the landscape of endometrial cancer diagnosis and treatment, researchers have identified two molecular targets that exhibit remarkable potential for nuclear theranostics—human epidermal growth factor receptor 2 (HER2) and cluster of differentiation 24 (CD24). Published recently in The Journal of Nuclear Medicine, this pivotal study delves into the promising domain of radiotheranostics, employing advanced positron emission tomography (PET) imaging probes to enhance detection accuracy and therapeutic targeting of endometrial tumors. The urgency behind this research stems from the rising incidence and mortality rates of endometrial cancer, the most prevalent gynecological malignancy worldwide, where existing treatment modalities for late-stage disease remain woefully insufficient.
Endometrial cancer typically responds well to surgical intervention in its initial stages, primarily through hysterectomy, which offers a high chance of remission. However, disseminated or recurrent forms pose a daunting clinical challenge due to the lack of effective molecularly tailored therapies. Conventional chemotherapies and radiation therapies tend to fall short either by limited efficacy or significant toxicity. Hence, the integration of molecular imaging with targeted agents—theranostics—stands as a beacon of hope for improving patient stratification, enabling personalized treatment regimens, and ultimately enhancing survival outcomes.
In pursuit of this goal, the investigative team embarked on an in-depth evaluation of three candidate biomarkers: HER2, mucin-16 (MUC16), and CD24. These antigens were selected based on their reported expression patterns in various cancers and their suitability as targets for molecular imaging and targeted radionuclide therapies. Employing immunohistochemistry and cell-based assays, the researchers assessed their expression in both healthy uterine/endometrial tissues and endometrial cancer-derived cell lines and patient tissues, providing a comprehensive comparative framework to identify differential overexpression amenable to nuclear medicine applications.
Central to this exploration was the generation of specialized immunoPET probes conjugated with Zirconium-89 (^89Zr), a positron-emitting radioisotope favored for its optimal half-life suited to antibody-based imaging. Specifically, ^89Zr-DFO-trastuzumab targeted HER2, ^89Zr-DFO-AR9.6 was directed against MUC16, and ^89Zr-DFO-ATG-031 targeted CD24. The design hinged on the principle that radiolabeled monoclonal antibodies selectively bind to their cognate antigens on tumor cells, enabling precise in vivo visualization and quantification through PET imaging.
Subsequent in vivo investigations utilized mouse models harboring subcutaneous xenografts developed from endometrial cancer cell lines as well as patient-derived xenografts (PDX). These murine models served as robust platforms to evaluate the biodistribution, tumor targeting efficiency, and imaging contrast of the radiotracers. Intriguingly, the CD24-targeted probe ^89Zr-DFO-ATG-031 consistently demonstrated the highest tumor uptake coupled with superior tumor-to-background ratios, highlighting its potential as a front-runner for radiotheranostic applications. Conversely, ^89Zr-DFO-trastuzumab exhibited moderate but nonetheless promising tumor localization, while the MUC16-targeting agent provided suboptimal imaging results, underscoring the heterogeneity of antigen accessibility and probe performance.
Mechanistically, CD24 is a glycosylphosphatidylinositol-anchored cell surface protein implicated in tumor progression and metastasis through modulation of cell adhesion and immune evasion pathways. Its overexpression in aggressive endometrial tumors may render it a valuable biomarker for both imaging and therapeutic intervention. HER2, a well-established oncogenic receptor tyrosine kinase, holds a legacy of clinical relevance in breast and gastric cancers; its emerging role in endometrial cancer introduces possibilities for repurposing trastuzumab-based therapeutic strategies augmented by diagnostic imaging.
The dual capability of these radiolabeled antibodies to identify tumor antigen expression non-invasively while simultaneously serving as vehicles for radionuclide therapy embodies the essence of theranostics—melding diagnostic precision with personalized treatment. PET imaging facilitates the selection of patients who express the target antigen at sufficient levels, thereby optimizing dosing and minimizing off-target effects. Therapeutically, these agents can be modified to deliver cytotoxic radioisotopes, such as alpha or beta emitters, directly to malignant cells, enabling targeted cellular destruction with limited systemic exposure.
Beyond the laboratory, the clinical translation of HER2 and CD24-targeted radiotheranostics bears significant implications. For patients with recurrent or metastatic endometrial cancer who currently face limited options, these strategies may offer new hope in terms of improved detection, therapy guidance, and real-time monitoring of treatment response. Moreover, the utilization of immunoPET probes can streamline drug development pipelines by providing robust biomarkers for therapeutic efficacy, expediting regulatory approvals.
The researchers emphasize that while MUC16 did not demonstrate encouraging imaging properties in this context, the comprehensive evaluation approach establishes a valuable template for future biomarker validation efforts. By integrating molecular biology, radiochemistry, and preclinical imaging, this study charts a course for systematic identification of viable radiotheranostic targets in understudied malignancies beyond the traditional scope.
Dr. Brian M. Zeglis, senior author and noted expert in nuclear chemistry, highlights the novelty and necessity of this approach in endometrial cancer. He stresses that advancing these radiotheranostic probes into clinical trials will require collaborative efforts spanning academia, industry, and regulatory bodies. Nevertheless, the promising preclinical data underscore the transformative potential of molecularly guided nuclear medicine techniques in addressing pressing unmet needs in oncology.
Such investigations align with the broader trend towards precision oncology, where therapeutics are tailored based on individual tumor biology rather than conventional histopathological classification. Leveraging PET imaging with radiolabeled antibodies not only refines diagnosis but also furthers understanding of tumor heterogeneity, receptor dynamics, and resistance mechanisms at a molecular level. This integrative paradigm could pave the way for iterative improvements in patient outcomes through adaptive treatment strategies.
In conclusion, the identification of HER2 and CD24 as robust radiotheranostic targets offers a new frontier in the molecular imaging and treatment of endometrial cancer. The study’s rigorous experimental design, coupled with insightful interpretation of imaging and biodistribution data, positions these molecular targets at the forefront of forthcoming clinical applications. As the quest for effective management of advanced endometrial cancer intensifies, such innovations herald a paradigm shift toward more precise, effective, and personalized nuclear medicine interventions.
Subject of Research: Animals
Article Title: Evaluating Radiotheranostic Targets for Endometrial Cancer
News Publication Date: September 4, 2025
Web References:
https://doi.org/10.2967/jnumed.125.270318
References:
Sebastiano et al., J Nucl Med 2025; jnumed.125.270318
Image Credits:
Sebastiano et al., J Nucl Med 2025; jnumed.125.270318
Keywords:
Cancer treatments, Biomarkers, Cancer