In a groundbreaking study from Texas A&M University, researchers have tapped into the realm of biomedical engineering by utilizing Ecoflex, a versatile silicone rubber, to develop highly realistic skin-like models. These innovations could significantly enhance our understanding of catheter-related infections, which pose serious risks in healthcare settings. Much like the painstaking processes employed by makeup artists in Hollywood, such as the dedicated team behind Jim Carrey’s transformation into the Grinch, this research reflects an intersection of art and science that holds great potential for public health.
The team’s research culminated in the formulation of Ecoflex-based replicas that closely simulate human skin properties, including texture, elasticity, and moisture levels. These characteristics are essential for accurately replicating the conditions under which bacterial infections typically arise. Their findings were published in the esteemed journal Scientific Reports, shedding light on a major advancement in the fight against healthcare-associated infections that frequently result from intravenous (IV) catheterization.
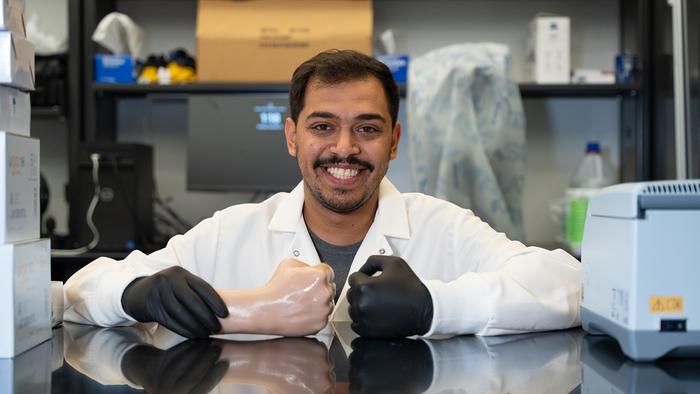
Notably, Majed Othman Althumayri, a graduate student and lead author of the study, emphasized the advantageous properties of Ecoflex. Its ease of use and rapid curing process means that it can be efficiently applied in laboratories without extensive protocols, making it an ideal material for research applications. This is particularly important when exploring infections caused by bacteria that inhabit human skin, mainly Staphylococcus epidermidis—one of the most prevalent microorganisms found on our bodies.
Statistically, the American healthcare system battles upwards of 80,000 catheter-related bloodstream infections every year in intensive care units alone. This staggering figure underscores the pressing need for effective solutions to contain and prevent these infections. Althumayri pointed out the slow pace of innovation in the realm of infection prevention strategies, suggesting that this delay may arise from the inadequacies in existing testing platforms for new catheter designs and biosensor technology training.
To tackle these challenges, the research team utilized Ecoflex 00-35 to create precise molds that mimic common IV insertion sites on the body, such as the forearm and elbow. The development of these molds involved the integration of artificial bones and tubes to simulate veins, resulting in detailed skin-like replicas. This methodological approach is not only innovative but also crucial for conducting realistic experiments that bridge laboratory conditions and clinical realities.
Upon constructing these models, the team undertook rigorous testing to assess key properties such as wettability and bacterial adhesion, alongside mechanical factors like elasticity. Their results showed extraordinary precision, with the Ecoflex models replicating human skin roughness with an impressive 7.5% error margin. High-resolution imaging further validated these findings, illustrating that bacteria could effectively adhere to and proliferate on these artificial skin surfaces.
A pivotal aspect of this investigation involved simulating an IV catheter insertion into the Ecoflex hand models. This crucial experiment illuminated the growth phases of bacteria, thus providing invaluable insights into the mechanisms underlying infection progression. The potential applications of these Ecoflex replicas stretch beyond merely studying existing medical practices; they could play a formative role in designing advanced catheter systems that minimize infection risks.
While the results are promising, researchers cautioned that the current study does not fully encapsulate the complexities of real-world scenarios encountered in hospitals. Dr. Hatice Ceylan Koydemir, the corresponding author and an assistant professor in the Department of Biomedical Engineering, reiterated the importance of developing realistic models that incorporate various physiological factors. She emphasized the necessity of future research to include elements like body fluids and diverse clinical situations to deepen the understanding of Ecoflex’s applicability in a medical context.
The collaborative effort in this research found support from prestigious institutions including the National Institute of General Medical Sciences, the U.S. Department of Defense, and the National Science Foundation-funded Engineering Research Center PATHS-UP. Such backing enriches the implications of their work, making strides toward more robust methodologies for infection prevention and treatment.
Furthermore, the Ecoflex’s biocompatibility stands as a testament to its potential in multiple biomedical applications, ranging from prosthetics to various device designs. The lightweight nature and adaptability of Ecoflex make it suitable for engineers looking to create devices that enhance patient safety and comfort. This multi-faceted utility could revolutionize practice across a variety of medical fields, advancing the overarching mission of improving patient outcomes.
With the promise of Ecoflex, researchers aim not only to study the risk factors associated with infections but also to address the broader implications for public health. The study is particularly critical as healthcare settings continue to grapple with the widespread impact of device-associated infections, highlighting the necessity for innovative solutions that can prevent harm to patients.
As the research continues to unfold, it paves the way for exciting advancements in the biomedical arena. It embodies a vibrant collaboration among graduate students and faculty that reflects a shared commitment to improving healthcare outcomes through innovative engineering solutions. The interdisciplinary nature of this work signifies a versatile approach to tackling some of healthcare’s most pressing challenges.
In conclusion, this pioneering work at Texas A&M University represents a merging of engineering acumen with clinical realities, fostering a new era in infection prevention strategies. The capacious potential of Ecoflex in modeling bacterial interactions stands to not only enhance laboratory studies but also inform real-world applications in medical device design. As researchers refine these models, the hope is that we might witness a significant reduction in hospital-acquired infections, thereby transforming the landscape of patient care in the near future.
Subject of Research: Biomedical applications of Ecoflex material
Article Title: Bioinspired skin-like in vitro model for investigating catheter-related bloodstream infections
News Publication Date: 30-Oct-2024
Web References: https://www.nature.com/articles/s41598-024-76652-y
References: DOI: 10.1038/s41598-024-76652-y
Image Credits: Credit: Emily Oswald/Texas A&M Engineering