Revolutionizing COPD Diagnosis: A Multidimensional Approach Integrating Imaging and Symptoms
Chronic obstructive pulmonary disease (COPD) remains a leading cause of morbidity and mortality worldwide, yet the paradigms governing its diagnosis have long relied almost exclusively on spirometric measures of airflow obstruction. This restrictive framework has increasingly been recognized as insufficient to capture the disease’s heterogeneous nature. In a landmark advancement reported in the Journal of the American Medical Association (JAMA), a team of researchers led by Surya Bhatt, M.D., from the University of Alabama at Birmingham, propose a transformative, multidimensional diagnostic schema for COPD—integrating computed tomography (CT) imaging and respiratory symptomatology alongside traditional lung function tests. This novel approach promises not only to refine diagnostic accuracy but also to stratify patients more effectively by their risk of adverse outcomes.
Spirometry has historically been the cornerstone for identifying COPD, focusing on the presence of airflow obstruction as evidenced by reduced ratios of forced expiratory volume in one second (FEV1) to forced vital capacity (FVC). However, reliance solely on lung function tests has its limitations. Many individuals with clinically significant structural lung abnormalities or symptomatic respiratory impairment present without overt spirometric obstruction, leading to underdiagnosis or misclassification. The new schema introduces an interplay between major and minor criteria, recognizing that COPD is a multidimensional disorder characterized by interplay between physiological changes, anatomical deterioration, and clinical symptoms.
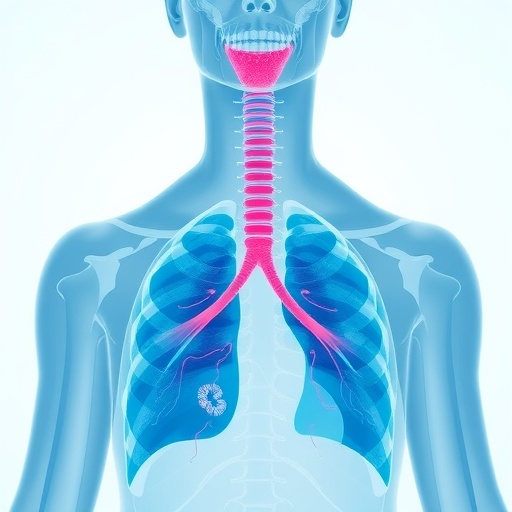
At the heart of this diagnostic model lies the major criterion—airflow obstruction confirmed by spirometry. Complementing this are minor criteria encompassing imaging biomarkers and symptom-based evaluations. CT imaging is utilized to detect emphysema, characterized by parenchymal destruction, and airway wall thickening—both hallmarks of COPD pathology. Concurrently, symptom-based criteria assess dyspnea, chronic bronchitic symptoms, and their impact on quality of life, capturing the clinical manifestation of disease burden beyond what spirometry can reveal. A patient fulfilling the major criterion plus at least one minor criterion qualifies for diagnosis, while in the absence of airflow obstruction or unavailable spirometric data, meeting three out of five minor criteria suffices.
This multidimensional approach was assessed across a robust cohort of 9,416 participants drawn from diverse clinical settings in the United States and Canada. The findings evidenced that individuals newly identified as having COPD through this schema bore a significantly heightened risk profile—including elevated all-cause and respiratory-specific mortality, accelerated decline in pulmonary function, and more frequent exacerbations—underscoring the clinical relevance of integrating imaging and symptoms in diagnosis. Equally notable is the exclusion, through this schema, of participants exhibiting airflow obstruction without corresponding symptoms or structural abnormalities, thus refining patient classification and potentially avoiding unnecessary treatment.
The implications of this paradigm shift extend broadly into clinical practice. COPD is notoriously heterogeneous, with phenotypic variability influencing prognosis and therapeutic responsiveness. By accommodating clinical diversity through multidimensional assessment, this diagnostic strategy aligns with precision medicine principles, offering tailored identification of at-risk patients. For clinicians, this means a more sensitive detection method, inclusive of those traditionally overlooked by spirometry-centric practices, enabling earlier intervention and more nuanced management.
CT imaging’s role in this framework deserves particular emphasis. Advanced imaging modalities afford unparalleled visualization of lung parenchyma and airway architecture. High-resolution computed tomography unearths subtle emphysematous changes and airway remodeling not discernible by standard pulmonary function tests. Inclusion of these objective structural markers propels diagnosis beyond physiological surrogates to anatomical confirmation, bridging a critical gap between clinical presentation and underlying pathology.
Symptom evaluation, as operationalized in this schema, addresses a pivotal clinical dimension often marginalized in COPD diagnosis. Respiratory symptoms—dyspnea, cough, sputum production—affect patient functionality and prognosis independently and may precede measurable airflow obstruction. Incorporating standardized symptom-based criteria formalizes their diagnostic value, recognizing patient-centered outcomes as integral to disease characterization. Such inclusion is anticipated to resonate with clinicians who have long relied on symptomatology alongside spirometry in practice, validating these assessments through an evidence-based framework.
The study’s authors, including co-senior authors Edwin K. Silverman and James D. Crapo, stress that although widespread adoption of this multidimensional approach portends improved diagnostic granularity, therapeutic implications require further empirical validation. Determining whether treatment modifications based on this schema translate into superior clinical outcomes is a critical next step. Nevertheless, the authors suggest this work lays vital groundwork for standardized operationalization of COPD diagnosis, guiding both research and clinical care.
An editorial commentary by Francesca Polverino, M.D., Ph.D., from Baylor College of Medicine lauds the study as a milestone, heralding a departure from the “overly dependent” spirometry-based diagnosis that has prevailed for decades. She underscores that the proposed model’s most groundbreaking aspect is its assertion that airflow obstruction is no longer mandatory for diagnosis—challenging entrenched dogma and embracing the disease’s multifaceted reality. This fresh perspective is germane in light of growing awareness that COPD encompasses a spectrum of pathological and clinical presentations.
The methodological rigor supporting this schema is anchored in a meta-analytic approach, synthesizing data from multiple cohorts to enhance generalizability and statistical power. The inclusion of 52 authors across 24 prestigious institutions underscores the collaborative and multidisciplinary nature of this endeavor, reflecting a consensus in the respiratory medicine community for advancing COPD diagnosis. The resultant criteria are thus not merely novel but well-vetted through extensive empirical scrutiny.
Technological advancements enabling this approach are emblematic of the broader integration of digital imaging and artificial intelligence in pulmonary medicine. Quantitative imaging biomarkers, emerging from sophisticated CT analysis and possibly augmented by machine learning algorithms, hold promise for enhancing diagnostic objectivity and reproducibility. These tools facilitate precise phenotyping, a crucial step for personalized therapeutic targeting in COPD, which notoriously resists one-size-fits-all treatment.
Given the global burden of COPD—affecting an estimated 392 million people worldwide—the impact of improved diagnostic criteria can be profound. Early and accurate identification of those at risk for rapid progression or severe exacerbations may prompt more aggressive preventive strategies, minimizing healthcare utilization and improving quality of life. Furthermore, better classification holds potential to refine patient selection in clinical trials, accelerating the development of novel therapeutics tailored to distinct COPD phenotypes.
While the study acknowledges that lung function testing remains a foundational element of diagnosis, it simultaneously calls for an expanded diagnostic lens. The model pragmatically leverages readily obtainable clinical data—symptom questionnaires and chest CT—tools increasingly accessible in tertiary and even secondary care settings. Such an inclusive framework could democratize COPD diagnosis and reduce disparities arising from underrecognition in symptom-only or spirometry-only approaches.
In summation, Dr. Bhatt and colleagues’ multidimensional diagnostic schema represents a paradigm shift in COPD identification, reflecting the nuanced interplay of airflow limitation, structural lung pathology, and symptom burden. This comprehensive approach holds promise to recalibrate both clinical and research strategies, fostering earlier detection, refined risk stratification, and ultimately, improved patient-centered outcomes. Its adoption signals a new era in respiratory medicine where diagnosis transcends simplistic spirometric thresholds to embrace the complexity and heterogeneity intrinsic to COPD.
Subject of Research: People
Article Title: A new multidimensional diagnostic approach for chronic obstructive pulmonary disease
News Publication Date: 18-May-2025
Web References: https://jamanetwork.com/journals/jama/fullarticle/2834253
References: Bhatt S, et al. “A new multidimensional diagnostic approach for chronic obstructive pulmonary disease.” JAMA. 2025; DOI:10.1001/jama.2025.7358
Image Credits: Credit: University of Alabama at Birmingham (UAB)
Keywords: Chronic obstructive pulmonary disease, Computerized axial tomography, Clinical imaging, Diagnostic imaging, Medical diagnosis