A groundbreaking global study has unveiled a critical yet preventable driver behind some of the most devastating complications associated with type 2 diabetes: physical inactivity. Researchers, analyzing data from over 2.3 million adults living with diabetes across diverse global regions, have demonstrated that failing to meet recommended physical activity levels—defined as at least 150 minutes per week of moderate-to-vigorous exercise—accounts for a substantial proportion of severe diabetes-related complications. Notably, up to 10% of strokes, diabetic retinopathy, and heart failure cases may be directly attributable to sedentary lifestyles.
The research fundamentally challenges the long-held perception that complications stemming from diabetes are an unavoidable consequence of the disease’s progression. Instead, it posits physical activity not only as a mitigating factor but as a core element in the prevention strategy against these debilitating outcomes. The findings emerge from a comprehensive analysis synthesizing population cohort studies, national health surveys, and rigorous meta-analyses, integrating global physical activity patterns in alignment with current World Health Organization guidelines.
From a mechanistic perspective, physical inactivity exacerbates insulin resistance, a hallmark of type 2 diabetes pathophysiology, thereby accelerating vascular damage and microvascular impairments. Macrovascular complications such as coronary heart disease and heart failure are similarly aggravated by the absence of adequate physical activity, primarily due to compromised endothelial function and heightened inflammatory processes. This study quantifies, for the first time, the population-attributable fractions (PAFs) for these critical conditions specifically linked to inactivity among diabetic populations, highlighting the tangible preventive potential that increased physical activity holds.
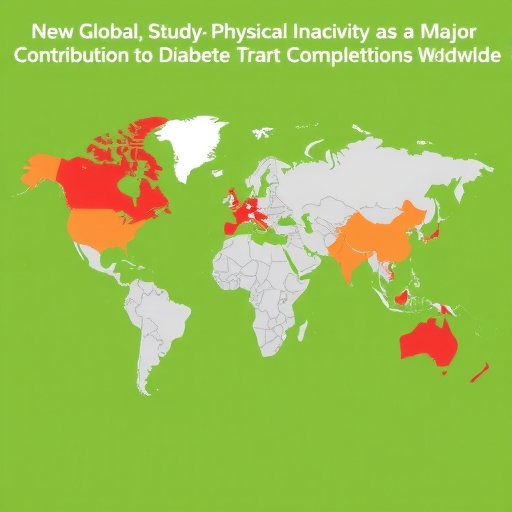
Intriguingly, the burden of inactivity-induced complications is not evenly distributed worldwide. Regionally, high-income Asia Pacific countries, Latin America, and parts of Central Asia, North Africa, and the Middle East exhibit the highest preventable burdens. This disparity underscores the interplay between socioeconomic factors, cultural norms, and infrastructural support for physical activity. Leisure-time physical activity remains dominant in high-income countries, whereas transport- and occupational physical activity are more prevalent in low- and middle-income regions, where barriers such as safety and urban design pose significant challenges.
The study also brings social inequities into sharp focus, identifying that women and individuals with lower educational attainment bear a disproportionate share of these preventable complications. Lower educational status often correlates with reduced health literacy, limited access to recreational spaces, and increased caregiving responsibilities, all acting as barriers to maintaining physical activity. These findings call for nuanced policy interventions that explicitly incorporate gender dynamics and educational disparities as central considerations in public health strategies.
Economic stratification within countries further compounds this complex landscape. Higher national income is associated with greater overall physical inactivity-attributable fractions, but marginalized groups within these nations suffer the majority of preventable consequences. This paradox highlights the need for policies that transcend average economic metrics and directly address within-country disparities by targeting vulnerable populations with tailored support programs.
The global diabetes epidemic now affects close to 590 million individuals worldwide, placing enormous pressure on health systems through direct costs related to the management of complications like cardiovascular disease, disability, and vision loss. The escalating economic burden intersects with an inevitable human toll in morbidity and premature mortality. Against this backdrop, the reframing of physical activity promotion as an indispensable pillar in alleviating healthcare demands represents a paradigm shift of considerable importance.
The study’s authors emphasize that a “one-size-fits-all” approach to physical activity prescription will fail to address the multifaceted realities across cultures and economies. Successful interventions must reconcile global evidence with localized context, accounting for varying forms of physical activity and distinct societal constraints. For instance, while urban infrastructure development may encourage walking and cycling in some regions, alternative strategies such as community-based exercise programs or workplace physical activity initiatives may be more effective elsewhere.
Integrating physical activity counselling into routine diabetes management protocols emerges as a critical recommendation. This requires training healthcare providers to prioritize behavioral interventions, supporting patients through motivational interviewing, personalized goal-setting, and ongoing monitoring. Moreover, national noncommunicable disease strategies must incorporate equity-focused frameworks that proactively dismantle barriers faced by women and socioeconomically disadvantaged groups to ensure inclusive access to physical activity opportunities.
The research team’s meticulous methodology, which combines international cohort data with meta-analytic risk estimates and global surveillance findings, strengthens the study’s validity and applicability. This robust evidence base offers policymakers and clinicians actionable insights, reinforcing physical activity not merely as general advice but as a potent, evidence-backed therapeutic tool to prevent the most severe consequences of diabetes.
In sum, this transformative study redefines the role of lifestyle interventions in diabetes care, elevating physical activity from an ancillary recommendation to a central preventive measure that can substantially reduce the global burden of diabetes complications. Given the disproportionate impact on vulnerable populations and the varying regional challenges, a concerted, multifaceted approach is imperative. Promoting physical activity equitably within diabetic populations can lead to significant gains in health outcomes, reductions in healthcare expenditure, and improvements in quality of life worldwide.
Subject of Research: People
Article Title: Global, regional, and national burden of major diabetes-related complications attributable to physical inactivity
News Publication Date: 14-Jan-2026
Web References: http://dx.doi.org/10.1016/j.jshs.2026.101123
Image Credits: Dr. Natan Feter from University of Southern California, United States
Keywords: Health and medicine, Human health, Public health, Human biology, Physical exercise, Human physiology, Diseases and disorders, Diabetes, Type 2 diabetes, Type 1 diabetes, Diabetic retinopathy, Retinopathy