Recent research has unveiled a transformative approach to understanding bone homeostasis, focusing on the interplay between the nervous system and skeletal health. The study, led by Liang, TZ, Jin, ZY, and Lin, YJ, showcases potential therapeutic avenues stemming from this nexus. Highlighting the importance of both the central and peripheral nervous systems, the researchers aim to bridge a significant gap in existing medical literature regarding the communication pathways that influence bone density and health. As we delve into the implications of these findings, it becomes clear that targeting neural influences on bone regulation may revolutionize treatment protocols in the future.
Historically, bone health was regarded predominantly through the lens of calcium metabolism and physical activity. The traditional understanding placed limited emphasis on the nervous system’s role in regulating bone turnover. Recent insights leverage advancements in neuroscience to reveal that bones are not merely structural entities but dynamic tissues influenced extensively by an intricate network of signals originating from the nervous system. This paradigm shift opens several unexplored pathways for therapies aimed at treating osteoporosis and related skeletal disorders more effectively.
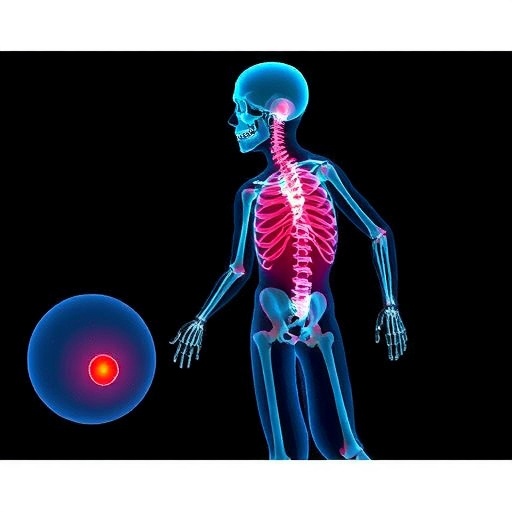
The authors’ investigation delineates the mechanisms through which both central and peripheral nervous systems contribute to bone regulation. Central nervous system factors include neural circuits originating from brain regions known to influence appetite and energy expenditure, which were previously underappreciated in their role concerning the skeletal system. Through pathways such as the sympathetic nervous system and parasympathetic responses, neural signaling evidently dictates osteoblast and osteoclast functions, balancing bone formation and resorption.
Among the peripheral components highlighted, sensory and sympathetic nerves within the bone marrow show surprising interactions with immune cells, significantly impacting bone remodeling processes. Calcium and phosphate levels, crucial for bone health, depend on efficient signaling between these neural factors and the endocrine system. By understanding these intricate communication patterns, the potential arises to create targeted interventions that can mitigate age-related bone loss or treat metabolic bone diseases.
Furthermore, the study posits that the collaboration between neurotrophic factors and bone-regulating hormones provides a fertile ground for pharmaceutical advancements. For instance, the role of brain-derived neurotrophic factor (BDNF) in promoting osteoblast function presents a promising target for drug developments. Leveraging the body’s own biological mechanisms rather than introducing foreign substances could result in fewer side effects and enhanced efficacy in treatments for bone pathologies.
The implications extend beyond merely therapeutic strategies; they suggest a holistic approach to patient care. Understanding the link between mental health, stress levels, and bone density could lead practitioners to adopt more comprehensive assessment and treatment frameworks. This psychosomatic relationship highlights that patients experiencing chronic stress or mental health disorders may also be at increased risk of weaker bones. Mental wellness could thus become an integral component of osteological health assessments.
Research also suggests that lifestyle factors, coupled with genetic predispositions, influence the nervous system’s effect on bone health. A sedentary lifestyle, for example, has been shown to negatively affect neurological signaling pathways, which in turn can lead to decreased bone density. Enabling patients to engage in more active lifestyles can serve as a preventive measure against osteoporosis, reinforcing the importance of exercise not only for muscle strength but for maintaining healthy bones through neurological health.
As therapeutic insights begin to unfold, the possibility of developing biomimetic drugs that mimic or enhance neuro-osteogenic factors gains traction. The exploration of natural compounds that can enhance nerve signaling to bones is an exciting frontier. Bioactive molecules found in certain foods or supplements could be harnessed to foster better communication between nervous and skeletal systems, heralding a new era of integrative medicine.
The researchers underscore the necessity of more comprehensive clinical trials to validate these mechanisms in human subjects. Observational studies that link neural health with bone density measurements could solidify the theoretical framework, leading to evidence-based practices that incorporate mental and neural health as integral to skeletal wellness. Moreover, understanding individual variance in response to treatment could spur personalized medicine approaches that cater to specific neurological profiles.
The potential for adversities from pharmacological treatments should not be overlooked. Analyzing how existing medications affect not just the bone directly, but also the neural pathways contributing to bone health, is imperative for clinicians. By identifying and mitigating potential side effects of commonly prescribed drugs, healthcare providers could enhance treatment efficacy while minimizing risks.
This multi-faceted approach to bone health, with an emphasis on the central and peripheral nervous systems, has far-reaching implications. It not only offers hope for more effective therapies in managing bone ailments but also champions a broader recognition of how interconnected our biological systems truly are. Advancements in neuroscience, combined with ortho-therapeutics, might just be the key to unlocking robust treatments for conditions that compromise skeletal strength.
In conclusion, Liang, TZ., Jin, ZY., and Lin, YJ. have paved the way for a paradigm shift in our understanding of bone health through their exploration of neurobiological mechanisms. Their findings not only challenge traditional models of bone treatment but also open a multidisciplinary avenue for future research. As academia continues to unravel the complexities of these interactions, the quest for optimal strategies to combat bone-related ailments is poised to benefit countless individuals at risk.
The potential for integration of these strategies into routine clinical practice echoes a growing trend in modern medicine: the move towards holistic, patient-centered care. By acknowledging the significant role of the nervous system in skeletal health, researchers and clinicians alike can work towards innovative therapies that harness the body’s natural systems for better health outcomes.
The horizon is bright for those suffering from bone diseases, and with further investigation into this fascinating intersection of neurology and orthopedics, we may soon witness the development of treatments that not only alleviate the symptoms but also address the root causes of bone-related disorders, fundamentally changing the landscape of orthopedic care.
Subject of Research: The influence of the central and peripheral nervous systems on bone homeostasis and potential therapeutic strategies.
Article Title: Targeting the central and peripheral nervous system to regulate bone homeostasis: mechanisms and potential therapies.
Article References:
Liang, TZ., Jin, ZY., Lin, YJ. et al. Targeting the central and peripheral nervous system to regulate bone homeostasis: mechanisms and potential therapies.
Military Med Res 12, 13 (2025). https://doi.org/10.1186/s40779-025-00600-8
Image Credits: AI Generated
DOI: 10.1186/s40779-025-00600-8
Keywords: Bone homeostasis, nervous system, osteoblast, osteoclast, neurotrophic factors, osteoporosis, therapeutic strategies, skeletal health, personalized medicine.