In the labyrinthine domain of psychiatric disorders, schizophrenia stands out not only for its profound impact on cognition and perception but also for the elusive complexity of its underlying neurobiology. Despite decades of research, definitive neural signatures and mechanisms responsible for its diverse clinical manifestations have remained stubbornly difficult to pinpoint. Now, a sweeping new synthesis of neuroimaging meta-analyses promises to illuminate the path forward, offering a refined, stage-specific map of brain alterations that may finally unravel some of schizophrenia’s biological mysteries.
This substantial undertaking, conducted by Magioncalda, Yadav, and Martino and recently published in Nature Mental Health, represents an unprecedented effort to aggregate and integrate findings from 50 high-resolution neuroimaging meta-analyses. The researchers meticulously analyzed studies employing various modalities—including gray matter morphometry, white matter integrity assessments, intrinsic brain activity measurement, and task-based functional MRI—to parse out consistent patterns of brain changes across different phases of schizophrenia, from prodromal symptoms to chronic illness.
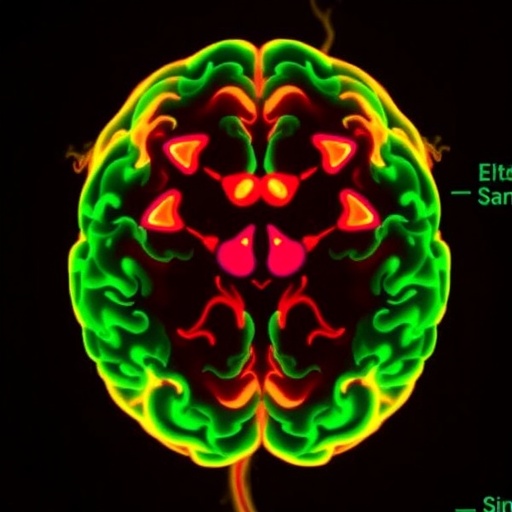
The first revelation of this exhaustive umbrella review is the recognition that schizophrenia-related brain alterations are not random nor static, but instead follow a coherent spatiotemporal progression. During the prodromal stage, when clinical symptoms first begin to emerge but before full-blown psychosis manifests, the most prominent disruption is gray matter atrophy concentrated in midline structures, notably the medial prefrontal cortex. This neural signature aligns with abnormalities in the central executive network, a system implicated in higher-order cognitive control and working memory—functions commonly impaired even in early illness stages.
As individuals transition to first-episode or early psychosis, the neuroimaging landscape becomes more complex and widespread. Additional cortical regions, especially within the operculum—comprising the insula, superior temporal gyrus, and neighboring cortices—show marked gray matter reductions. Alongside these cortical deficits, white matter disruptions emerge predominantly in fronto-temporal tracts adjacent to the lateral ventricles, including critical fiber bundles such as the fornix, cingulum, and long-range fasciculi. These changes coincide with dysfunction in the default-mode network (DMN), a brain network instrumental in self-referential thought and internal mentation, suggesting a neural substrate for the emergence of psychotic symptoms.
In chronic and deteriorative phases of schizophrenia, neuroanatomical alterations become more profound and widespread. The thalamus and lateral prefrontal cortex experience notable structural and functional impairments, reflecting the progressive nature of the disease. The thalamus, as a critical relay hub facilitating communication between cortical and subcortical structures, when compromised, potentially contributes to the pervasive deficits in sensory integration and cognitive coordination characteristic of longstanding schizophrenia.
One of the critical clinical correlates emerging from this synthesis is the relationship between opercular damage and hallmark symptoms such as auditory hallucinations. Structural impairment in the superior temporal gyrus, home to the auditory cortex, shows a robust association with the frequency and severity of hallucinations, highlighting a biological substrate for these typically distressing experiences. Meanwhile, dysfunction in the DMN has been linked not just to hallucinations but also to delusions, underscoring the network’s role in disrupted self-processing and aberrant salience attribution—a key feature in psychosis.
Notably, the authors propose that these neurobiological alterations may be specific to the prototypical form of schizophrenia, hinting at the heterogeneous nature of the disorder and raising important questions about the overlap and divergence among schizophrenia spectrum disorders and other psychotic illnesses. This specificity potentially offers a framework for tailoring interventions based on precise brain network disruptions, which could herald advances in biomarker-driven diagnosis and treatment.
Beyond mere cataloging, Magioncalda and colleagues integrate these findings into a comprehensive conceptual framework linking the spatiotemporal progression of brain changes with pathophysiological mechanisms and clinical phenomenology. This model posits that early medial prefrontal cortex deficits and central executive dysfunction precipitate the initial prodrome, while subsequent damage in opercular and fronto-temporal networks catalyzes the transition to psychosis. Chronic disease stages reflect accumulated thalamic and lateral prefrontal cortex pathology, underpinning sustained cognitive and functional decline.
Technically, the umbrella review distinguishes itself through its multi-dimensional approach. By pooling differing neuroimaging modalities and focusing on meta-analytically derived data rather than isolated single studies, the analysis markedly enhances statistical power and reliability. This approach helps overcome longstanding inconsistencies and contradictions that have marred previous efforts, providing the psychiatric neuroscience community with a robust and nuanced neurobiological account.
The implications of this work extend beyond academic curiosity. A clearer delineation of brain alterations tied to discrete illness phases suggests prospects for stage-specific biomarkers, where neuroimaging could serve as a prognostic and diagnostic tool. For example, detecting medial prefrontal cortex deficits early in at-risk individuals might allow targeted preventive strategies before psychosis onset, potentially modifying the disease course.
Moreover, understanding the networks implicated in specific symptoms opens the door to novel therapeutic interventions, such as noninvasive brain stimulation aimed at the insula or superior temporal gyrus to mitigate hallucinations, or neuromodulation of the DMN to reduce delusional thinking. This brain-centric precision medicine approach represents a paradigm shift in how schizophrenia might be conceptualized and treated in the near future.
The synthesis also underscores the importance of white matter disruptions in schizophrenia pathophysiology, a relatively underappreciated aspect until recent decades. The identified damage in major fasciculi not only explains deficits in inter-regional communication critical for cognitive and emotional processing but also highlights potential targets for therapies aimed at restoring white matter integrity, for instance via myelin repair strategies.
Further, this review brings to light the thalamus as a major nexus in chronic schizophrenia pathology. Traditionally overshadowed by cortical studies, the recognition of thalamic involvement aligns with emerging theories that schizophrenia is fundamentally a disorder of distributed neural circuits, not localized brain regions. This reframing promotes broader investigation into subcortical contributions to psychiatric illness and may inspire innovative multi-level approaches to study and treat these disorders.
Importantly, the authors acknowledge the heterogeneity in schizophrenia’s clinical presentation and underlying biology, which complicates universal biomarker identification and intervention design. However, by isolating a prototypical set of alterations, this research offers a foundation on which future stratification of patients could be based, potentially enabling personalized medicine in psychiatry—a field that has traditionally lagged behind other medical disciplines in this regard.
The umbrella review elegantly weaves together the complex tapestry of schizophrenia neurobiology, highlighting how structural and functional brain changes evolve from subtle prodromal deficits to extensive, chronic impairments. It moves the field toward a more integrated understanding that bridges neuroimaging data with clinical phenomenology, offering hope that the tangled biology of schizophrenia can be progressively unraveled.
As neuroscientists and clinicians grapple with the heterogeneity and clinical complexity of schizophrenia, this comprehensive meta-analytic framework serves as an invaluable roadmap, charting the dynamics of brain networks implicated in disease course and symptomatology. Future research building on these insights promises to refine diagnostic criteria, personalize treatment protocols, and ultimately improve outcomes for millions worldwide affected by this devastating disorder.
With its multi-modal, multi-cohort scope and its thoughtful synthesis, this umbrella review ushers in a new era of schizophrenia research, where big data meets clinical neuroscience. By illuminating the intricate neuroanatomical and functional progression underlying psychosis, it lays a critical foundation for the breakthroughs needed to transform mental health care.
Subject of Research: Schizophrenia neurobiology and brain alterations across illness stages, studied via meta-analyses of neuroimaging data.
Article Title: An umbrella review of neuroimaging studies and conceptual framework linking pathophysiology and psychopathology in schizophrenia.
Article References:
Magioncalda, P., Yadav, A. & Martino, M. An umbrella review of neuroimaging studies and conceptual framework linking pathophysiology and psychopathology in schizophrenia. Nat. Mental Health (2025). https://doi.org/10.1038/s44220-025-00493-5
Image Credits: AI Generated