As the prevalence of single-parent households continues to climb globally, a pressing concern has emerged regarding the mental health and emotional wellbeing of children raised in such family structures. Recent research spearheaded by a team including Y. Liao, X. Deng, and J. Gong offers a groundbreaking perspective into this discourse. Their extensive study, involving a massive cohort of over 49,000 upper elementary school students in China, employs network analysis to delve into the intricate web of depressive symptoms experienced by children from single-parent and two-parent families.
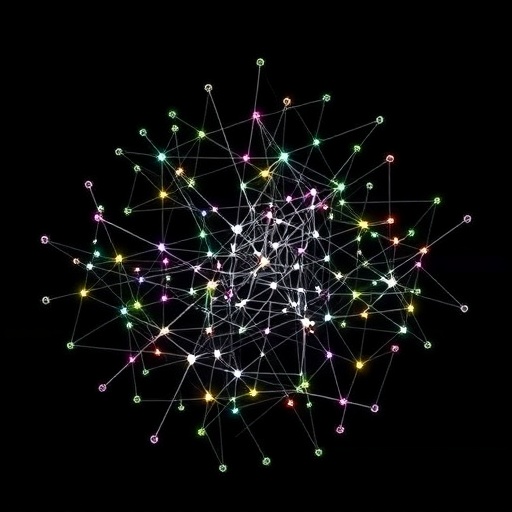
Traditional approaches to understanding depression in children often look at symptoms in isolation or by aggregate severity scores. However, network theory posits that symptoms themselves interact, forming complex interrelations that can influence the onset and maintenance of depressive states. This methodological innovation allows researchers to identify the most influential symptoms—referred to as “central symptoms”—which could serve as critical targets for intervention. By applying this lens, the study goes beyond surface-level comparisons, unearthing nuanced differences in symptom connectivity and prominence tied to family structure.
The research was conducted over a two-month period in late 2022 in Nanchong, located in Sichuan Province of China. The participants, numbering 49,109, were surveyed using the well-established Center for Epidemiological Studies Depression Scale (CES-D), a tool widely recognized for its reliability in assessing depression-related symptomatology in youth populations. This robust sample size, coupled with validated measurement instruments, lends substantial statistical power and credibility to their findings.
Analytically, the study employed the NetworkComparisonTest (NCT), a sophisticated statistical approach designed to compare network structures and strengths between groups. This allowed for a direct juxtaposition of depressive symptom networks among children from two different familial conditions: two-parent versus single-parent households. Additionally, the study explored differences between children from single-father and single-mother environments, recognizing potential variations driven by the parent’s gender.
One of the standout revelations from the study was the distinct centrality of symptoms within each group. For children living in two-parent households, the symptom labeled “Sad” showed the greatest centrality, signifying its pivotal role in shaping and sustaining the depression network. In contrast, the top central symptom for children from single-parent families was “Not enjoying life,” highlighting a divergence in the internal emotional landscape based on family composition. Such distinctions imply that depressive experiences are not uniformly manifested across family dynamics; rather, they are intricately shaped by the psychosocial contexts in which children are reared.
Notably, the density of connections between symptoms—referred to as global strength—was significantly higher in the networks corresponding to single-parent families. With a global strength score of 8.50 compared to 8.11 in two-parent family networks and a corresponding p-value of 0.02, these findings suggest higher symptom interconnectivity. Heightened network density may indicate more entrenched or self-reinforcing depressive patterns, suggesting single-parent children could face greater challenges in breaking depressive cycles without targeted intervention.
The symptom “Restless sleep” emerged as particularly noteworthy with increased centrality in single-parent families. This heightened prominence, confirmed by a strength difference of 0.12 with an adjusted p-value of 0.01, points toward sleep disturbances as a key feature of depression in these children. Sleep problems have been widely documented in psychiatric literature as both symptom and risk factor for depression, and this research underscores the need to pay closer attention to sleep quality within family-tailored mental health strategies.
Intriguingly, when the symptom networks of children from single-mother and single-father families were compared, differences in global strength and overall network architecture were not statistically significant. This suggests that regardless of whether a child is raised by a mother or father alone, the depressive symptomatology they experience shares similar structural profiles, emphasizing the broader psychosocial challenges linked to single-parenthood rather than the specific parent’s gender.
The implications of this research extend beyond clinical diagnosis to the realm of practical intervention design. By identifying central symptoms that vary with family structure, mental health practitioners can direct their efforts more precisely. For example, interventions for children from single-parent households might prioritize boosting life enjoyment and addressing sleep problems, while approaches for two-parent family children might focus more on alleviating pervasive sadness.
Beyond clinical settings, these insights contribute to a more refined understanding of how family environments influence childhood mental health. They emphasize the importance of acknowledging diversity within the population of depressed children, reinforcing that effective mental health care demands bespoke solutions rather than a one-size-fits-all model. Policymakers and educational authorities could utilize such findings to advocate for tailored preventive and support programs targeted at vulnerable family groups, potentially mitigating the burden of childhood depression at a community or national level.
Furthermore, the use of network analysis in this context exemplifies how advanced computational tools can revolutionize psychological research. By moving away from traditional linear models and embracing symptom interconnectivity, this study captures the dynamic and multifaceted nature of depression. This approach opens avenues for future research exploring other moderating factors such as socioeconomic circumstances, parental mental health status, or cultural influences in shaping these symptom networks.
The study’s scale and methodological rigor mark a significant stride in global child mental health research. Its extensive sample size, rooted in a comprehensive screening program, provides a rare window into depressive symptoms from a population-level perspective. The findings underscore the necessity for mental health frameworks that integrate family structure considerations to optimize early detection and intervention pathways.
In summation, this pioneering investigation reveals fundamental differences in how depressive symptoms organize and interact within children from single-parent compared to two-parent families. Highlighting the centrality of “Not enjoying life” and “Restless sleep” in the former, and “Sad” in the latter, alongside denser symptom networks in single-parent contexts, it challenges existing paradigms around childhood depression and advocates for tailored therapeutic approaches. As childhood depression remains a critical public health issue worldwide, such innovative insights are invaluable for crafting more effective, sensitive, and impactful mental health interventions.
Subject of Research: Network analysis of depressive symptoms among children from single-parent and two-parent families
Article Title: A large-sample (N = 49,109) network analysis of depressive symptoms in children from single-parent and two-parent families
Article References:
Liao, Y., Deng, X., Gong, J. et al. A large-sample (N = 49,109) network analysis of depressive symptoms in children from single-parent and two-parent families. BMC Psychiatry 25, 999 (2025). https://doi.org/10.1186/s12888-025-07435-6
Image Credits: AI Generated