In a monumental step forward in the battle against pancreatic cancer, researchers have unveiled a pioneering clinical trial that combines a mutant KRAS-targeted vaccine with dual checkpoint blockade immunotherapy. This phase I trial, recently published in Nature Communications, sheds new light on potential therapeutic strategies for one of the deadliest malignancies, offering renewed hope for improved outcomes in patients following surgical resection of pancreatic tumors.
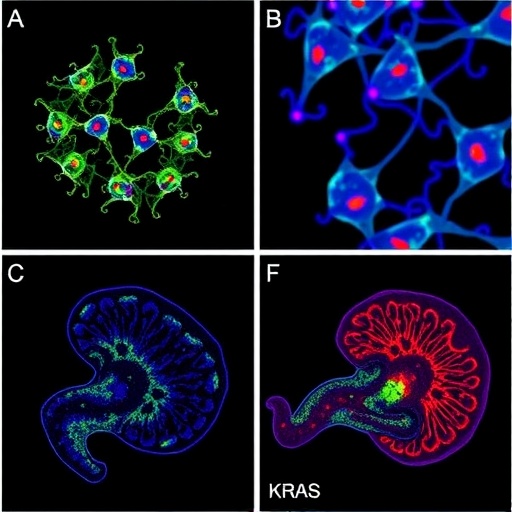
Pancreatic adenocarcinoma remains a formidable challenge in oncology due to its aggressive nature and poor prognosis. The notorious resilience of pancreatic cancer cells to conventional therapies has driven scientists to explore innovative approaches rooted in immunotherapy. At the heart of this particular study lies the mutant KRAS gene, which is mutated in approximately 90% of pancreatic tumors, making it an ideal molecular target for personalized cancer vaccines.
The mutant KRAS vaccine constitutes a novel peptide-based immunogen specifically designed to elicit a robust cytotoxic T-cell response against cancer cells harboring this mutation. By training the immune system to recognize the aberrant peptide fragments derived from mutant KRAS proteins, the vaccine aims to prompt targeted destruction of residual cancer cells that often fuel relapse after surgical intervention.
However, the tumor microenvironment in pancreatic cancer notoriously suppresses immune responses through multiple checkpoint pathways, effectively “putting the brakes” on T-cell activity. To counter this immune inhibition, the researchers incorporated dual checkpoint blockade therapy targeting both PD-1 and CTLA-4—two critical immune inhibitory receptors. This dual blockade strategy is hypothesized to unleash T cells’ full cytotoxic potential, thereby synergizing with the vaccine-induced anti-KRAS immune response.
Eighteen patients with completely resected pancreatic cancer participated in this phase I clinical trial. The inclusion criteria focused on individuals with high-risk tumor profiles, emphasizing those with detectable KRAS mutations. Over the course of treatment, patients received a series of vaccine doses combined with checkpoint inhibitor infusions, with careful monitoring for safety, immunogenicity, and initial indications of clinical benefit.
Safety was the primary endpoint, and impressively, the combination regimen demonstrated a manageable toxicity profile. Most adverse events were low grade, with fatigue and mild skin reactions being the most commonly reported. Importantly, no dose-limiting toxicities were observed, paving the way for further investigation in larger cohorts.
Immunological assessments revealed that the mutant KRAS vaccine elicited a potent T-cell response in the majority of treated patients. Binding assays confirmed the expansion of KRAS-specific CD8+ T cells, which were further potentiated in the context of dual checkpoint inhibition. Functional analyses demonstrated enhanced production of key effector cytokines such as interferon-gamma, indicating an activated immune milieu capable of targeting residual tumor cells.
Additionally, longitudinal monitoring indicated a favorable modulation of the tumor microenvironment. Blood and tissue samples showed decreased levels of regulatory T cells and myeloid-derived suppressor cells, both known to dampen anti-tumor immunity. This shift likely results from the combined checkpoint blockade, which disrupts immunosuppressive signaling pathways and may create a more permissive environment for the vaccine-primed T cells to operate.
One of the most compelling findings was the identification of increased infiltration of cytotoxic CD8+ T cells in post-surgical tumor margins—a location where minimal residual disease frequently seeds recurrence. This reinforces the vaccine and immunotherapy combination’s potential to provide a vigilant immunological barrier, reducing the likelihood of tumor relapse.
While the trial was not designed to measure long-term efficacy or survival outcomes, preliminary observations suggest a trend toward improved disease-free survival intervals compared to historical controls. Though these early results are encouraging, larger phase II and III trials will be essential to conclusively determine the clinical benefit and durability of this therapeutic strategy.
Mechanistically, this study represents an important confluence of personalized cancer vaccination and immune checkpoint blockade. The precision targeting of mutant KRAS epitopes harnesses tumor-specific antigens, while simultaneous inhibition of PD-1 and CTLA-4 checkpoints addresses systemic immune suppression—a dual-pronged approach that might be pivotal in overcoming pancreatic cancer’s historically refractory nature.
Moreover, these findings could have significant implications beyond pancreatic cancer. KRAS mutations are prevalent in several other malignancies, including colorectal and lung cancers, suggesting that similar vaccine and checkpoint blockade combinations might be extrapolated to these tumor types, thereby broadening the scope of impact.
Technological advances in peptide synthesis, adjuvant engineering, and immune monitoring underpinned this trial’s success. The ability to generate highly specific mutant KRAS peptides capable of inducing robust immune responses marks a noteworthy achievement in cancer vaccine technology, while dual checkpoint inhibitors have become a cornerstone of modern immunotherapy regimens.
Future research directions will undoubtedly focus on optimizing vaccine delivery platforms, dosing schedules, and identifying biomarkers predictive of responsiveness to combined immunotherapy. This will facilitate patient stratification and refinement of treatment protocols to maximize therapeutic efficacy while minimizing toxicity.
In conclusion, this groundbreaking phase I trial represents a testament to the rapidly evolving landscape of pancreatic cancer treatment. By strategically combining a mutant KRAS-specific vaccine with dual immune checkpoint blockade, researchers have demonstrated a promising avenue to enhance anti-tumor immunity in a disease long characterized by its resistance to therapy. These advances hold substantial promise in the quest to transform pancreatic cancer from a fatal diagnosis into a manageable condition.
As the oncology community awaits further validation through larger trials, this innovative approach stimulates hope and exemplifies the power of precision immunotherapy. The integration of molecularly targeted vaccines with immune-modulatory agents signals a new era in cancer treatment—one where tailored immune strategies might finally tip the scales against formidable foes like pancreatic cancer.
Subject of Research: Mutant KRAS-targeted vaccine combined with dual checkpoint blockade immunotherapy in resected pancreatic cancer
Article Title: Mutant KRAS vaccine with dual checkpoint blockade in resected pancreatic cancer: a phase I trial
Article References:
Huff, A.L., Haldar, S.D., Gergis, A.A. et al. Mutant KRAS vaccine with dual checkpoint blockade in resected pancreatic cancer: a phase I trial. Nat Commun 17, 1538 (2026). https://doi.org/10.1038/s41467-026-68324-4
Image Credits: AI Generated