In a pioneering case report published in the esteemed journal BMC Psychiatry in 2025, researchers have detailed a multidisciplinary approach to initiating clozapine treatment in a patient diagnosed with schizophrenia and comorbid autism spectrum disorder (ASD). This report sheds light on a challenging clinical scenario where standard antipsychotic regimens failed, and the introduction of clozapine demanded cautious and tailored strategies due to the patient’s unique neurodevelopmental profile.
Schizophrenia and autism spectrum disorder are complex conditions, each characterized by distinct but sometimes overlapping symptomatology. The intersection of these disorders introduces a layer of complexity not only in diagnosis but also in therapeutic management. Psychosis, a hallmark of schizophrenia, often shares qualitative symptom overlap with ASD, which complicates clinical interpretation and treatment choices. The co-morbidity rate is significant, thereby necessitating research into approaches that address both conditions concurrently.
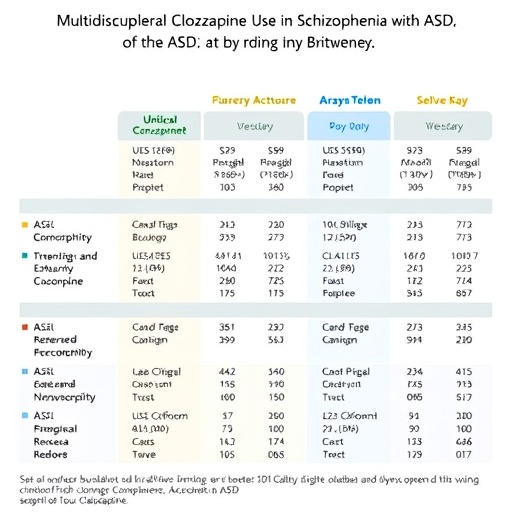
One major challenge clinicians face in treating such patients is the variable response to antipsychotic medications. While clozapine remains the gold standard for treatment-resistant schizophrenia, its use in individuals with ASD is fraught with concerns. Notably, these patients may be at an increased risk of adverse effects, including agranulocytosis, metabolic syndrome, and seizures, which makes prescribing clozapine a nuanced decision requiring enhanced vigilance and multidisciplinary cooperation.
The case under discussion highlights a patient suffering from persistent psychotic symptoms unresponsive to multiple antipsychotics. After conventional options failed, the treating team considered clozapine, recognizing its potential efficacy in treatment-resistant cases. However, the presence of comorbid ASD mandated a bespoke treatment plan, incorporating psychiatric, neurological, and behavioral expertise to mitigate risks and monitor the patient’s response meticulously.
Integral to this approach was the comprehensive assessment of the patient’s baseline neurocognitive functions, behavioral patterns, and physiological status. The team employed advanced neuropsychological evaluations combined with continuous hematological and metabolic monitoring to preempt potential adverse reactions. Such an integrative methodology ensured that clozapine treatment could be safely initiated, balanced against the backdrop of heightened vulnerability intrinsic to ASD.
The initiation phase was marked by a gradual titration of clozapine dosage, carefully tailored to minimize side effects while optimizing therapeutic impact. The multidisciplinary team worked collaboratively to adapt environmental stimuli and daily routines to the patient’s sensory sensitivities, which are often heightened in ASD. This environmental adjustment was crucial to enhance medication adherence and reduce anxiety-related exacerbations.
Throughout the treatment process, psychopharmacologists worked in tandem with behavioral therapists and caregivers, adjusting strategies based on longitudinal assessments of symptomatology and overall functioning. This fluid and dynamic configuration underscores the importance of multidisciplinary frameworks when addressing cases where psychiatric and neurodevelopmental disorders converge.
Remarkably, the patient demonstrated significant improvement in psychotic symptoms with clozapine, suggesting that despite the inherent risks, meticulous implementation of clozapine in patients with schizophrenia and ASD is feasible. This finding supports a growing consensus that therapeutic guidelines should be flexible and patient-centered, especially in cases with overlapping neuropsychiatric presentations.
Moreover, the case report calls attention to a critical gap in clinical research: the limited data on clozapine’s safety and efficacy within the ASD population. It emphasizes the urgent need for more extensive clinical trials and longitudinal studies designed specifically to explore pharmacotherapeutic responses and side effect profiles in this subgroup.
The successful outcome observed in this patient provides a proof of concept for the benefits of multidisciplinary integration in psychopharmacology. It champions the adoption of holistic care models that not only focus on symptom suppression but also prioritize patient quality of life, functional recovery, and the minimization of treatment-emergent complications.
In conclusion, this remarkable case offers a roadmap for psychiatrists and allied health professionals navigating the complex interface of schizophrenia and ASD. It advocates for personalized medicine guided by collaborative expertise and rigorous monitoring, ultimately expanding the therapeutic horizons for a demographic that has historically been challenging to treat effectively.
This publication is a vital contribution to psychiatric literature, stimulating discourse and innovation in the management of comorbid neuropsychiatric disorders. It exemplifies how tailored interventions, grounded in robust multidisciplinary approaches, can transform clinical outcomes even in the most challenging cases.
Subject of Research: Schizophrenia treatment in a patient with comorbid autism spectrum disorder using a multidisciplinary approach to clozapine initiation.
Article Title: A multidisciplinary approach to establishing clozapine in a patient with schizophrenia and comorbid ASD: a case report
Article References:
Bridges, M., Secchi, A., Whiskey, E. et al. A multidisciplinary approach to establishing clozapine in a patient with schizophrenia and comorbid ASD: a case report. BMC Psychiatry (2025). https://doi.org/10.1186/s12888-025-07280-7
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12888-025-07280-7