Majority of Medicaid Managed Care Plans Provide Coverage for Naloxone, But Access Barriers Remain
A recent comprehensive study emerging from Boston University School of Public Health reveals that nearly all Medicaid managed care plans (MCPs) in 40 states and Washington, D.C. include coverage for at least one formulation of naloxone, the critical opioid overdose reversal drug. Despite this widespread coverage, nuances such as restrictions on quantity and prior authorization requirements continue to impose significant obstacles for Medicaid recipients striving to obtain this life-saving medication. These findings, published in JAMA Network Open, represent the first large-scale assessment of naloxone coverage specifically within Medicaid managed care frameworks, which enroll approximately 80% of the Medicaid population—over 70 million individuals.
Naloxone, commonly known by the brand name Narcan, received U.S. Food and Drug Administration (FDA) approval for over-the-counter (OTC) sales in 2023, marking a milestone in public health efforts to expand access to overdose reversal treatments. Nevertheless, the OTC availability does not guarantee affordability; the average retail cost remains around $45 for a standard two-dose package, creating a substantial barrier for low-income individuals. Medicaid recipients are disproportionately affected by the opioid crisis, with overdose death rates twice that of the national average, making insurance coverage for naloxone an essential intervention in harm reduction strategies.
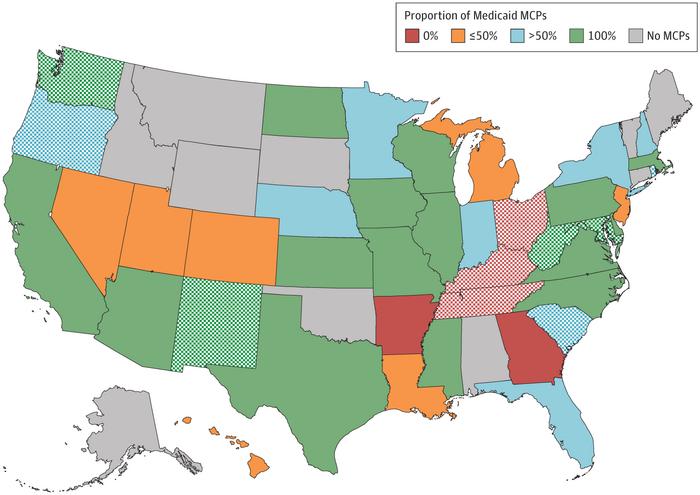
The observational study involved meticulous review of preferred drug lists (PDLs) from 264 Medicaid managed care plans covering more than 65 million enrollees. These PDLs determine the pharmaceutical agents favored by insurers, often dictating drug access through negotiated rebates and formularies. Researchers evaluated coverage across all naloxone formulations available: generic injectable, generic and brand 4-mg nasal sprays, and the newer, higher-dose 8-mg brand nasal spray. The data revealed that 94% of plans included coverage for at least one generic injectable or 4-mg nasal spray variant, with 91% covering both injectable and nasal spray formulations in generic or brand forms.
Despite widespread inclusion in formularies, the study highlighted persistent limitations imposed by many plans in the form of quantity limits, prior authorizations, or other utilization management tools. Such restrictions may prevent individuals from acquiring sufficient naloxone supplies, particularly in states experiencing high overdose rates. Notably, three states—Ohio, Kentucky, and Tennessee—reported Medicaid managed care plans that do not cover any form of naloxone, a concerning gap given these states’ elevated opioid mortality rates. While these associations do not establish causation, they underscore the critical need for policy interventions to promote broader, unencumbered access to naloxone in high-risk regions.
Lead author Sage Feltus, a research associate at BUSPH’s Department of Health Law, Policy & Management, emphasized the practical implications of these findings. She noted that although OTC naloxone availability marks progress, cost barriers remain formidable without insurance coverage. The high overdose mortality among Medicaid beneficiaries intensifies the demand for low-friction, affordable naloxone access through managed care plans. Feltus advocates for policy strategies such as eliminating prior authorization demands and unifying preferred drug lists to mandate coverage of all naloxone formulations, thereby reducing bureaucratic hurdles for providers and patients alike.
The study situates itself within the evolving landscape of the opioid crisis, which witnessed a disturbing surge in overdose deaths during the COVID-19 pandemic before preliminary data indicated substantial declines from 83,140 deaths in 2023 down to 54,743 in 2024. Naloxone’s role as the cornerstone of harm reduction is undisputed, capable of rapidly reversing the respiratory depression caused by opioids like fentanyl, heroin, and oxycodone. Despite long-standing efforts by public health officials and the U.S. Surgeon General to amplify awareness and availability, access disparities persist, particularly among vulnerable populations reliant on Medicaid.
One layer of complexity identified by the researchers involves the management of formularies at the intersection of state policies and insurer practices. More than half of plans were governed by state-defined preferred drug lists, yet these state-level mechanisms often correlated with lower coverage rates of generic injectable naloxone. This paradoxical finding suggests administrative complexities and potentially variable state Medicaid policies contribute to inconsistent naloxone accessibility. The study calls for further investigation into how insurer and state policy dynamics influence real-world access and outcomes.
Importantly, the study’s coauthors—including Dr. Maureen Stewart, a research associate professor at BUSPH, Dr. Jeffrey Bratberg from the University of Rhode Island College of Pharmacy, and doctoral trainee Sophia Balkovski from Brandeis University—stress the necessity of ongoing research to quantify the impact of coverage parameters on health outcomes among Medicaid recipients. While the presence of coverage is a foundational step, the effect of quantity restrictions and utilization management on overdose reversal rates remains underexplored and warrants in-depth study.
Advocates and policymakers are urged to interpret these findings as a clarion call for targeted reforms. Extending uniform coverage policies across states, minimizing administrative barriers such as prior authorizations, and ensuring adequate supply limits for naloxone can significantly enhance the ability of high-risk populations to effectively utilize this medication. As the opioid epidemic continues, evidence-based policy design integrating insights from studies like this becomes indispensable to curbing overdose morbidity and mortality.
The study also illuminates broader implications for health equity and the economics of drug access. Medicaid recipients, as a socioeconomically disadvantaged group, face compounded challenges from both the opioid epidemic and the intricacies of managed care insurance frameworks. This confluence underscores the importance of embedding naloxone coverage policies into a larger context of comprehensive addiction treatment and social support services to optimize public health impact.
Boston University School of Public Health, founded in 1976 and ranked among the world’s top public health institutions, reinforces its commitment to policy-oriented research with studies such as this. By scrutinizing the intersection of health law, policy, and pharmacoeconomics, the research team contributes critical data to inform reforms necessary for tackling one of America’s gravest public health emergencies.
In conclusion, while the landscape of Medicaid managed care naloxone coverage presents a largely positive picture of inclusion, substantive barriers still hinder equitable access. Coordinated efforts by states, managed care plans, and federal agencies are essential to dismantle these obstacles. The expansion of affordable, unrestricted access to naloxone remains a vital component of the national effort to prevent opioid overdose deaths and save lives.
Subject of Research: People
Article Title: Medicaid Managed Care Naloxone Coverage and Management
News Publication Date: June 27, 2025
Web References:
- FDA OTC Naloxone Approval: https://www.fda.gov/news-events/press-announcements/fda-approves-first-over-counter-naloxone-nasal-spray
- Overdose Deaths Data: https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2025/20250514.htm
- Surgeon General’s Advisory on Naloxone: https://www.hhs.gov/surgeongeneral/reports-and-publications/addiction-and-substance-misuse/advisory-on-naloxone/index.html
References:
- Feltus, S., Stewart, M., Bratberg, J., Balkovski, S. Medicaid Managed Care Naloxone Coverage and Management. JAMA Network Open. 2025. DOI: 10.1001/jamanetworkopen.2025.12866.
Image Credits: Boston University School of Public Health
Keywords: Opioids, Psychoactive drugs, Heroin, Drug abuse, Drug costs, Health care costs, Health care, Drug research, Insurance, Health insurance, Human health, Public health