In the ever-evolving landscape of orthopedic medicine, one innovation shines brightly in the realm of bone regeneration: the use of three-dimensional (3D) printing technology paired with innovative algorithms. Recent advancements illustrate that with the aid of Finite Element Analysis (FEA) and cell differentiation algorithms, medical professionals can now make significant strides in early-stage predictions of bone regeneration. The research conducted by Liu, Chan, and Huang establishes a groundbreaking methodology for modeling and application in complex fractures, particularly the dorsal double-plating in distal radius fractures.
Bone regeneration is a vital topic in orthopedic studies, especially in fractures that do not heal correctly or involve significant loss of bone mass. Traditional methods of assessing bone healing often relied on subjective assessments and radiographic evaluations, which may not accurately reflect the underlying biological processes. The incorporation of FEA allows for a more quantitative analysis of biomechanical environments, enabling researchers to simulate how different conditions affect bone regeneration. This advancement could revolutionize how orthopedic surgeons plan and execute treatment strategies.
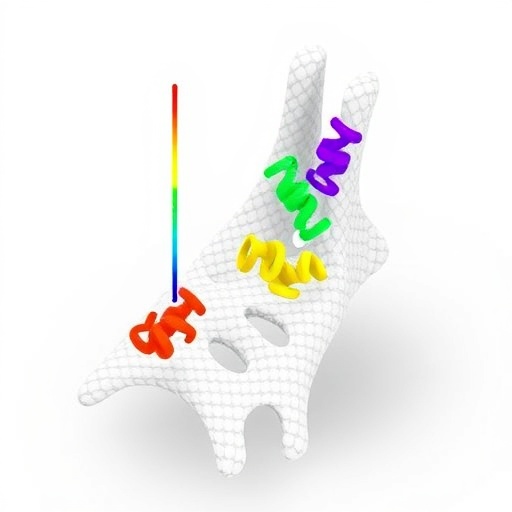
3D-printed scaffolds made from biocompatible and biodegradable materials like Poly(Lactic Acid) (PLA) and Polycaprolactone (PCL) provide a structural framework for cell proliferation and differentiation. These materials are not only affordable but can also be tailored to mimic the mechanical properties of natural bone. This characteristic is essential because it allows implanted scaffolds to withstand the mechanical loads experienced by bones in their native environments, thereby enhancing the chances of successful bone regeneration.
Moreover, the synergy between 3D printing and computational modeling techniques like FEA offers an exciting frontier in regenerative medicine. These technologies facilitate not just the design of the scaffolds but also their analysis under different physiological conditions. Liu and colleagues have taken a step towards harnessing these technologies effectively by developing a framework that integrates both FEA and cell differentiation insights to predict healing outcomes.
In their study, the researchers created digital twins of patients’ anatomical features, complete with detailed information on the fracture site. Through this simulation, they can assess how tissues will respond to various mechanical loads over time and predict how quickly and effectively the bone will regenerate. Such predictive modeling could be transformative for pre-operative planning, allowing surgeons to tailor treatments based on individual healing trajectories.
The implications of this research extend far beyond the operating room. For orthopedic surgeons, having a reliable forecast of healing can inform choices regarding surgical techniques, the material of the implants, and post-operative rehabilitation protocols. Furthermore, it means less trial and error in the treatment process, potentially reducing the overall time to recovery for patients dealing with complex fractures.
Additionally, the ability to produce patient-specific scaffolds via 3D printing opens a world of possibilities in personalized medicine. Custom-fit scaffolds that cater specifically to the individual’s anatomy could lead to improved integration between the scaffold and natural bone tissue. This personalized approach not only optimizes outcomes but also enhances patient satisfaction, as individuals are armed with treatment plans that consider their specific conditions.
As Liu et al. demonstrated, leveraging algorithms to simulate cellular behavior in conjunction with mechanical conditions represents the next frontier of regenerative medicine. By integrating these advanced techniques, the research not only showcases the utility of modern technology in medicine but also emphasizes the importance of interdisciplinary approaches. For example, combining insights from biology, engineering, and computer science can yield solutions that were previously unimaginable, setting a precedent for collaborative endeavors in the healthcare industry.
Moreover, the focus on early-stage prediction offers a compelling advantage in areas like trauma care and emergency medicine, where timely interventions can significantly affect outcomes. As medical professionals can anticipate issues before they manifest, proactive measures can be taken to ensure proper healing occurs, thus minimizing the risks of complications or the need for additional surgeries.
In conclusion, the research led by Liu, Chan, and Huang heralds a new dawn in orthopedic interventions. By merging advanced computational technology with cutting-edge material science, they present a model that not only enhances bone healing predictions but also creates a pathway towards more effective and personalized patient care. This burgeoning field has the potential to redefine how orthopedic practices approach bone regeneration, signifying a leap forward in both technology and patient health outcomes.
The evidence is compelling: as we continue to unravel the complexities of bone healing through innovative technologies, we are poised to usher in an era where surgery becomes more precise, recovery transforms, and patient outcomes improve dramatically. It’s a brave new world for regenerative medicine, driven by the fusion of technology, biology, and innovative thinking. This research leaves us anticipating further advancements that can bridge gaps in understanding regeneration and optimization of orthopedic care.
Subject of Research: Early stage prediction of bone regeneration using FEA and cell differentiation algorithms with 3D-printed PLA and PCL scaffolds.
Article Title: Early stage prediction of bone regeneration using FEA and cell differentiation algorithms with 3D-printed PLA and PCL scaffolds: modeling and application to dorsal double-plating in distal radius fractures.
Article References:
Liu, H.C., Chan, YH., Huang, SF. et al. Early stage prediction of bone regeneration using FEA and cell differentiation algorithms with 3D-printed PLA and PCL scaffolds: modeling and application to dorsal double-plating in distal radius fractures. 3D Print Med 11, 30 (2025). https://doi.org/10.1186/s41205-025-00278-7
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s41205-025-00278-7
Keywords: Bone regeneration, 3D printing, Finite Element Analysis, PLA, PCL, orthopedic surgery, personalized medicine, computational modeling, cell differentiation.