Out-of-hospital cardiac arrest (OHCA) represents a critical and often fatal medical emergency that claims a staggering number of lives around the world each year. Despite advances in emergency response and medical technology, approximately 90% of OHCA cases end in death, underscoring the urgent need to enhance prediction, prevention, and treatment strategies. The abrupt loss of cardiac function in these patients leads to an immediate cessation of blood circulation, and survival rates plummet by approximately 10% with each passing minute that defibrillation or advanced medical care is delayed. This grim reality has driven an interdisciplinary team of researchers at the University of Michigan to pioneer a novel approach leveraging machine learning to better understand and predict the risk factors associated with OHCA.
Traditional epidemiological models have primarily focused on well-known individual clinical risk factors, such as hypertension, coronary artery disease, and diabetes. While these remain essential for patient assessment, they fall short in accounting for the dynamic and external influences that may precipitate cardiac arrest events outside hospital settings. The new study, published in the esteemed journal npj Digital Medicine, pushes beyond these limitations by integrating a wide array of environmental and social variables with patient data. By harnessing the power of advanced machine learning algorithms, the researchers successfully identified 17 key factors that affect the likelihood of OHCA occurrences, opening promising avenues for proactive emergency response planning and public health interventions.
Central to the research is the utilization of an extensive dataset derived from the Cardiac Arrest Registry to Enhance Survival (CARES), the largest national database tracking out-of-hospital cardiac arrests. With an impressive sample size exceeding 190,000 cases spanning from 2013 to 2017, the team was well-equipped to train a robust predictive model capable of handling complex, nonlinear interactions among numerous variables. This computational approach surpasses the constraints of conventional linear regression models, which often struggle with multicollinearity and inability to capture intricate temporal and spatial fluctuations in data related to environmental factors.
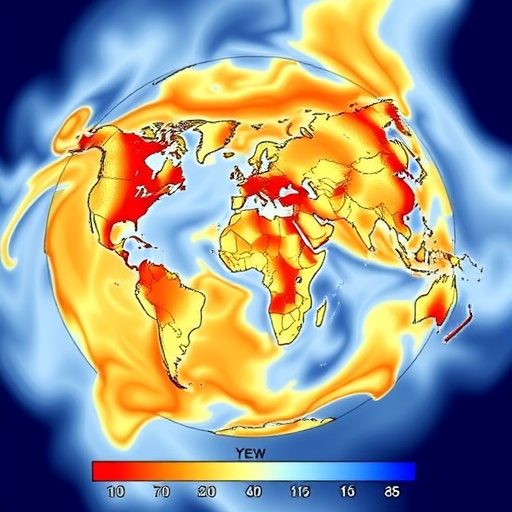
One of the most notable findings relates to ambient weather conditions. The analysis revealed that both unusually cold temperatures and extreme heat days are strongly correlated with spikes in OHCA incidence. Relative humidity also emerged as a significant determinant, influencing the physiological stress placed on the cardiovascular system. These findings echo and extend previous epidemiological observations, illuminating how rapid weather variability may act as a potent external stressor triggering cardiac events. The exact biological mechanisms remain under investigation, but hypotheses suggest that abrupt temperature changes can induce vasoconstriction, blood pressure fluctuations, and heightened inflammatory responses, all of which exacerbate cardiac vulnerability.
Critically, social determinants such as poverty and racial composition were shown to amplify the impact of adverse weather conditions. This intersection highlights the importance of considering socioeconomic context alongside environmental triggers, as communities with limited access to healthcare resources or those experiencing systemic inequities bear disproportionate burdens of OHCA risk. The model’s incorporation of these multifaceted factors marks a paradigm shift in cardiovascular risk assessment, moving toward a more holistic understanding of how external environments and social structures converge to influence health outcomes.
What sets this machine learning model apart is its high prediction accuracy and its capacity to forecast OHCA patterns up to seven days in advance. This temporal foresight is crucial for emergency medical services, enabling them to strategically allocate resources, optimize ambulance deployments, and potentially reduce response times which are pivotal for improving survival rates. Such an anticipatory framework could transform emergency readiness from a reactive to proactive posture, ultimately saving lives by ensuring that help arrives faster where and when it is most needed.
Despite these promising advances, the researchers emphasize ongoing challenges. The model performs best in areas actively participating in the CARES registry, where rich and consistent data enable precise prediction. In regions lacking comprehensive data, predictive accuracy diminishes, underscoring the need for more widespread data collection and integration. Moreover, the mechanisms by which rapid weather shifts precipitate cardiac arrest remain incompletely understood, necessitating further multidisciplinary studies involving physiology, meteorology, and social sciences. Enhancing patient-level granularity and integrating wearable device data could further refine the model’s predictive capabilities.
The study’s implications extend beyond emergency response logistics. Public health agencies stand to benefit immensely by merging this predictive tool with real-time weather forecasts. Such integration could power targeted alert systems that warn vulnerable populations—including elderly individuals and those with preexisting cardiovascular conditions—about impending high-risk days. Educational campaigns tailored to community-specific risk profiles can reinforce preventive behaviors, such as hydration, avoidance of strenuous outdoor activity, and timely medication adherence during periods of adverse environmental conditions.
The project, led by Dr. Takahiro Nakashima and colleagues at the University of Michigan, also underscores the critical role of collaborative international support. Funded by institutions including the Japan Society for the Promotion of Science and the Takeda Science Foundation, this cross-disciplinary effort exemplifies global commitment toward addressing cardiovascular emergencies through innovative technology. The research team advocates for expanded partnerships to incorporate diverse demographic and geographic data, thereby enhancing the model’s universality and equity.
Looking forward, the integration of environmental data with patient-specific clinical profiles signifies a new frontier in cardiovascular risk stratification. As machine learning techniques continue to evolve, their potential to untangle complex health determinants and provide actionable insights will grow exponentially. The convergence of big data analytics, environmental science, and emergency medicine promises not only to reduce mortality from OHCA but also to inspire a broader reimagining of how healthcare systems anticipate and respond to acute health threats on a population scale.
This transformative study not only redefines our understanding of OHCA risk but also charts a path toward smarter, data-driven healthcare strategies that can adapt to the changing climate and societal landscape. Delivering timely, precise predictions of cardiac arrest incidents has profound implications for saving lives, optimizing healthcare resources, and empowering communities worldwide to mitigate one of the deadliest medical emergencies known to humanity.
Subject of Research: People
Article Title: Development and evaluation of a machine learning model predicting out-of-hospital cardiac arrest using environmental factors.
News Publication Date: 22-Dec-2025
Web References:
10.1038/s41746-025-02235-4
Keywords: Health and medicine