In a groundbreaking study published in the Journal of Ovarian Research, researchers led by Qi, L., Yao, X., and You, X. have shed light on the intricate dynamics of microvascular density in advanced ovarian cancer patients. This research is particularly significant as it explores the impact of neoadjuvant chemotherapy augmented with or without the addition of the monoclonal antibody, bevacizumab. By focusing on a real-world setting, the authors offer insights that may bridge the gap between clinical trials and everyday treatment scenarios, positioning their findings within a context that is profoundly relevant for both medical professionals and patients alike.
Ovarian cancer remains a leading cause of cancer-related morbidity and mortality among women worldwide. Its insidious nature frequently leads to advanced stages at the initial diagnosis, which poses daunting treatment challenges. Prior to this study, much of the existing literature has primarily concentrated on clinical trial findings. However, Qi et al.’s study diverges from this norm by utilizing real-world data that captures the nuances of patient diversity and clinical practice variability. This approach offers a more comprehensive understanding of how treatments perform outside controlled experimental environments.
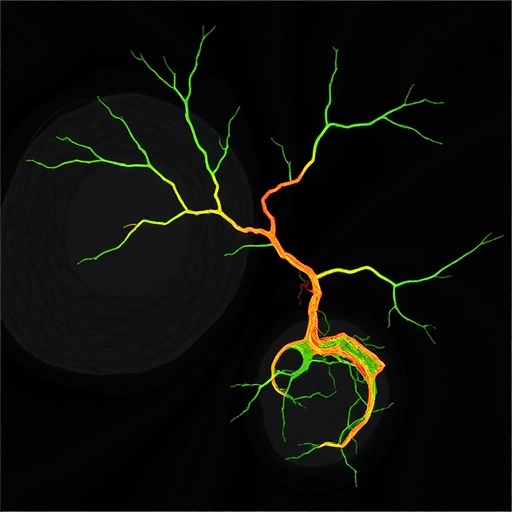
Microvascular density, a critical parameter in understanding tumor angiogenesis, has garnered increasing attention in cancer research. It reflects the extent of blood vessel formation within tumors, which is vital for facilitating tumor growth and metastasis. High microvascular density is often associated with poor prognoses in several cancers, including ovarian cancer. By examining the differences in microvascular density before and after neoadjuvant chemotherapy, especially with the introduction of bevacizumab, the researchers aim to elucidate the drug’s efficacy in altering tumor vascular characteristics, which could have profound implications for patient outcomes.
The study involved a cohort of patients diagnosed with advanced ovarian cancer, all of whom underwent neoadjuvant chemotherapy regimens that were comparable except for the presence of bevacizumab in half of the cases. By applying rigorous histopathological techniques, the researchers measured microvascular density using methods such as immunohistochemistry. This meticulous approach allowed for accurate quantification of the density of blood vessels within the tumor microenvironment, establishing a critical link between treatment administration and vascular response.
One of the pivotal findings of this study was the elucidation of how bevacizumab influences microvascular density. The administration of bevacizumab, an agent that inhibits vascular endothelial growth factor (VEGF), resulted in a notable reduction in microvascular density when compared to chemotherapy alone. VEGF plays a crucial role in promoting angiogenesis, and its blockade appears to disrupt the tumor’s ability to sustain its vascularization, leading to potential regression in tumor growth rates. These findings could alter established treatment paradigms, suggesting that integrating bevacizumab with neoadjuvant chemotherapy may enhance therapeutic effectiveness.
Additionally, the study examined heterogeneity in microvascular responses among different patients, highlighting that individual variations might influence treatment outcomes. These differences underscore the need for personalized treatment strategies that consider the biological and genetic make-up of tumors. Advancements in precision medicine hold promise for tailoring therapies that align better with individual patient profiles, ultimately enhancing treatment efficacy and reducing adverse effects.
While the authors provided compelling evidence supporting the use of bevacizumab, they also emphasized the importance of monitoring potential side effects, particularly in the context of a comprehensive treatment plan. Previous studies have highlighted concerns regarding increased risks of complications such as bleeding, bowel perforations, and hypertension when using anti-VEGF therapies. These risks underscore the necessity for a cautious approach, ensuring that benefits outweigh potential detriments in individualized management plans.
Moreover, the implications of this research extend beyond mere academic interest; they resonate deeply with clinical practice and can directly impact patient management strategies. Healthcare providers may need to reassess treatment options based on an improved understanding of tumor dynamics. For patients diagnosed with advanced ovarian cancer, this study offers a glimmer of hope, indicating that strategic modifications in therapy may lead to improved clinical outcomes.
In conclusion, the study conducted by Qi and colleagues stands as a crucial step forward in understanding the vascular behavior of advanced ovarian cancer. The findings highlight the importance of integrating real-world evidence with clinical practices, paving the way for further investigations to solidify the role of vascular targeting therapies. With ongoing advancements in treatment modalities, continued research is essential to explore the full potential of optimizing patient outcomes through personalized medicine approaches.
As the medical community absorbs these insights, it is evident that future studies will need to expand upon these findings. Investigating the long-term effects of microvascular modulation and its subsequent impact on overall survival rates in ovarian cancer patients will be an important frontier in this field. Moreover, the potential of incorporating various multimodal therapies alongside vascular-target therapies warrants rigorous exploration to achieve better therapeutic efficacy and patient quality of life.
This research not only adds to the growing body of knowledge surrounding ovarian cancer treatment but also underscores the critical role of microvascular dynamics in cancer biology. The promise of enhancing therapeutic strategies based on such fundamental understandings could revolutionize the landscape of cancer care, one patient at a time.
As we anticipate future developments in oncology, the integration of innovative therapies, such as bevacizumab, opens new avenues of hope for patients grappling with advanced ovarian cancer. The meticulous work conducted by Qi and colleagues serves as a potent reminder of the power of scientific inquiry and its potential to translate into tangible benefits for patients worldwide.
Ultimately, this study urges a shift in perspective within the oncology community—encouraging a focus not only on traditional chemotherapy but also on innovative approaches that target the underlying mechanisms of tumor growth. Such a shift could signify a monumental change in the prognosis for those affected by ovarian cancer, heralding an era of improved treatment paradigms and patient outcomes.
Subject of Research: Advanced Ovarian Cancer and Microvascular Density
Article Title: Analysis of microvascular density differences in advanced ovarian cancer after neoadjuvant chemotherapy with or without bevacizumab in real world.
Article References:
Qi, L., Yao, X., You, X. et al. Analysis of microvascular density differences in advanced ovarian cancer after neoadjuvant chemotherapy with or without bevacizumab in real world.
J Ovarian Res (2025). https://doi.org/10.1186/s13048-025-01923-9
Image Credits: AI Generated
DOI:
Keywords: Microvascular Density, Advanced Ovarian Cancer, Neoadjuvant Chemotherapy, Bevacizumab, Angiogenesis, Vascular Targeting, Personalized Medicine, Clinical Outcomes, Precision Medicine.