Microplastics, ubiquitous microscopic particles originating from the breakdown of larger plastic debris, have emerged as significant environmental contaminants, infiltrating ecosystems and the human food chain alike. Their insidious presence in our environment has raised alarms among researchers and public health officials alike. As the research evolves, one particularly alarming hypothesis is taking center stage: microplastics could be an emerging driver of osteoarthritis, a debilitating joint condition that affects millions worldwide. This theory, explored in depth by Malik et al., necessitates serious consideration given the implications for public health.
At first glance, the connection between microplastics and osteoarthritis may appear tenuous; however, recent research suggests otherwise. Microplastics accumulate not just in oceans and soils, but also present in the air we breathe and the food we consume. The quantities in which these particles are found are alarming, suggesting that human exposure could be significant. With the flexible and durable nature of plastics, the breakdown process can result in tiny particles remaining in the environment far longer than one might expect. Understanding how these particles interact with biological systems is critical, as it could reveal insights into chronic conditions such as osteoarthritis.
Researchers point to the potential for microplastics to serve as vectors for harmful chemicals and pathogens, which could exert detrimental effects on joint health. Many plastics contain additives and are treated with chemicals during their lifecycle—substances known to disrupt endocrine functions or promote inflammatory responses. Preliminary laboratory studies have shown that exposure to microplastics can provoke inflammatory pathways in human cells, hinting at a biological mechanism that could link plastic exposure to joint degeneration.
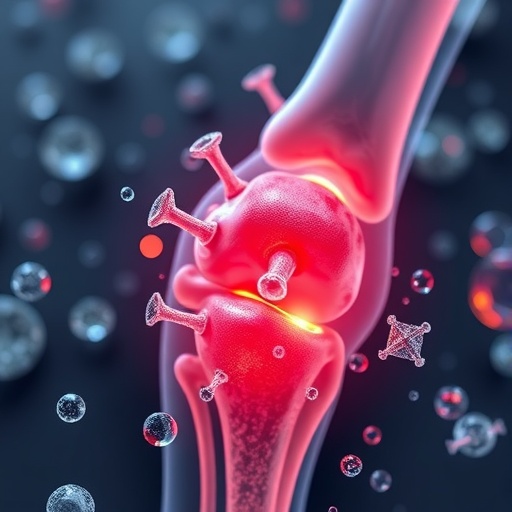
Osteoarthritis, primarily characterized by the degeneration of cartilage and underlying bone in joints, often stems from a combination of genetic, mechanical, and environmental factors. With an emerging focus on lifestyle and environmental influences in its etiology, the hypothesis connecting microplastics to this condition deserves earnest attention. As the prevalence of arthritis rises across the globe, particularly among the aging population, the inquiry into potential environmental triggers like microplastics becomes ever more vital.
To better understand this phenomenon, Malik and colleagues have synthesized existing research, correlating data on environmental exposures and incidences of osteoarthritis onset. Their translational approach emphasizes the need to analyze microplastics not only in isolation but also in conjunction with other known risk factors, providing a multi-faceted view of joint disease development. The findings suggest that increasing levels of exposure could exacerbate inflammatory responses, ultimately leading to cellular damage in cartilage.
The implications of these emerging insights extend far beyond laboratory findings; they point towards a societal call to action. Awareness of the potential health hazards associated with microplastics could reshape public perceptions of plastic use and waste. Education on the sources and exposure pathways of microplastics can instigate lifestyle changes that help mitigate individual risk, while fostering advocacy for policy changes aimed at reducing plastic pollution.
As researchers dive deeper into the mechanics of this connection, gaps remain in the current understanding that warrant further investigation. For example, longitudinal studies on populations with varying levels of microplastic exposure could provide rich data on the development of osteoarthritis over time. Similarly, exploring the interaction between microplastics and genetic predispositions will be critical in devising comprehensive models for predicting health outcomes.
In this pursuit of knowledge, inter-disciplinary collaborations will be vital. Environmental scientists, toxicologists, public health experts, and rheumatologists must work hand-in-hand to dissect the causal relationships implicated in this emerging health crisis. The development of standardized methods to measure microplastic exposure in human populations while analyzing its bioaccumulation in tissues can provide essential details needed for future interventions.
As the scientific community continues to unravel the complexities of the relationship between environmental toxins and chronic diseases, it becomes clearer that actions must be taken to limit plastic waste. Stakeholders, from policymakers to manufacturers, must be engaged in creating sustainable practices that diminish the prevalence of plastics in our environment. The public’s growing understanding of toxic pollutants could accelerate shifts toward eco-friendlier industries that prioritize human and ecological health over convenience.
Moreover, integrating knowledge about microplastics into medical education can enhance healthcare outcomes. Raising awareness among practitioners regarding the environmental determinants of health can support proactive strategies for patient care. As clinicians become more knowledgeable about the links between microplastics and conditions like osteoarthritis, timely interventions could help alleviate some of the disease’s burdens on individuals and healthcare systems.
Equipped with the latest findings, the conversation surrounding osteoarthritis must evolve from focusing solely on traditional risk factors to embracing a broader view that includes environmental exposures. The potential relationship between microplastics and chronic joint conditions like osteoarthritis emphasizes the urgency of addressing plastic pollution on both individual and societal levels.
In conclusion, as research like that of Malik et al. progresses, we must not only remain vigilant regarding the potential health risks posed by microplastics but actively advocate for systemic changes. The fight against plastic pollution is not solely an ecological endeavor; it is intrinsically tied to human health. By illuminating the connections between environmental toxins and chronic disease, we can inspire a healthier future, free from the pervasive influences of synthetic pollutants. Collectively, the quest for answers in the laboratory signals the beginning of a broader societal transformation toward sustainable living.
Subject of Research: Microplastics and osteoarthritis
Article Title: Microplastics as an emerging driver of osteoarthritis: a translational synthesis of environmental exposure, patho-mechanisms, and public health implications.
Article References:
Malik, M.A., Wu, S., Zhang, W. et al. Microplastics as an emerging driver of osteoarthritis: a translational synthesis of environmental exposure, patho-mechanisms, and public health implications.
J Transl Med 23, 1061 (2025). https://doi.org/10.1186/s12967-025-07081-2
Image Credits: AI Generated
DOI:
Keywords: microplastics, osteoarthritis, environmental exposure, public health, inflammation, chronic disease, plastic pollution.