A groundbreaking meta-analysis recently published in the journal Medicina reveals that Transcendental Meditation (TM) is a remarkably potent intervention for reducing symptoms of post-traumatic stress disorder (PTSD) across a broad spectrum of populations and trauma types. This comprehensive review synthesizes findings from 15 rigorous studies involving over 1,200 participants from diverse ethnicities and backgrounds, demonstrating not only the efficacy but also the rapid onset of therapeutic benefits associated with TM practice. The implications of this research signal a transformative shift in how clinicians and public health practitioners might approach PTSD treatment in the future.
PTSD, a debilitating disorder resulting from exposure to traumatic events, presents a persistent challenge to mental health care worldwide. Traditional therapies often demand patients to confront their traumatic experiences directly, an approach that can exacerbate symptoms and deter engagement. Transcendental Meditation, in contrast, offers a non-trauma-focused, non-pharmacological alternative that calms the nervous system without requiring direct confrontation with distressing memories. This meta-analysis evidences the clinical power of TM, pegging its average effect size at 1.01. Given that effect sizes above 0.80 are considered large and clinically significant, TM’s performance stands out as exceptionally robust in the PTSD treatment landscape.
Examining the global applicability of TM, the studies encompassed participants from countries including the United States, Japan, the Democratic Republic of Congo, Ukraine, South Africa, Israel, and Australia. The trauma types affecting these individuals varied widely—from war veterans grappling with combat-related trauma to survivors of domestic violence, refugees displaced by conflict, healthcare workers overwhelmed during the COVID-19 pandemic, and even prison inmates dealing with past violence and systemic oppression. Across every demographic and trauma etiology, TM proved consistently effective, reducing PTSD symptom scores by at least 10 points on the PTSD Checklist (PCL), a threshold widely recognized as clinically meaningful.
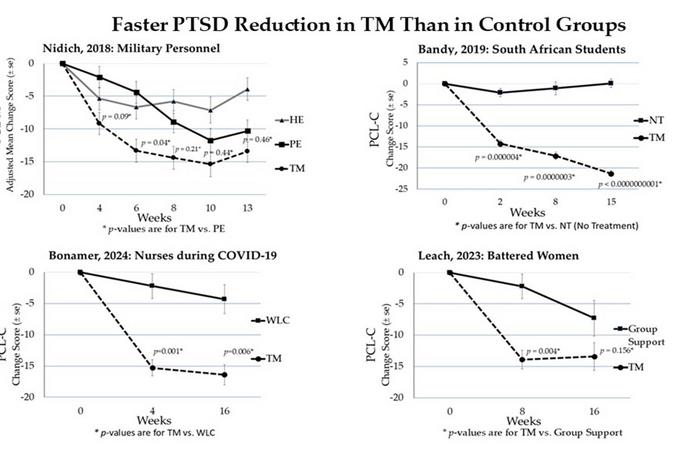
What sets TM apart in this meta-analysis is not only its broad efficacy but also the speed at which it exerts therapeutic effects. All fifteen studies reported that TM practitioners experienced faster symptom reduction compared to control groups receiving standard care or other interventions. In some cases, such as military personnel studied by Nidich et al. (2018), TM outperformed conventional first-line therapies like Health Education and Prolonged Exposure therapy. Similarly, South African college students traumatized by war and racial discrimination saw more rapid improvements than students receiving no treatment. Nurses studying TM during the height of the COVID-19 pandemic also reported quicker PTSD symptom relief compared to waitlist controls, a vital finding given the acute stress faced by healthcare workers during public health crises.
The mechanistic underpinnings of TM’s efficacy in PTSD are increasingly supported by cutting-edge biomedical research. A companion study, also referenced in Medicina, elucidates how TM influences stress-related molecular pathways, including the modulation of cortisol levels, electrophysiological brain activity (EEG), and gene expression profiles linked to stress response and cognitive function. These physiological changes foster resilience and recovery, potentially mitigating not only PTSD symptoms but also associated cardiometabolic risks and neurodegenerative processes tied to chronic stress. The integration of neurobiological and psychological findings positions TM as a uniquely holistic intervention with both immediate symptomatic and long-term systemic benefits.
In parallel, prior comparative meta-analyses that included other meditation forms underscore TM’s superiority in PTSD symptom reduction. While general meditation modalities demonstrated a moderate average effect size (0.67), TM showed a notably larger effect (1.13 in the December 2024 study), highlighting its distinct efficacy profile. This suggests that the standardized TM technique, characterized by effortless mental repetition of a mantra, may engage neural circuits and autonomic regulation differently than mindfulness or other meditative practices, leading to more profound clinical improvements.
The testimonial accounts of frontline practitioners add a compelling real-world dimension to the scientific data. Colonel (Ret.) Brian Rees, M.D., a co-author and former U.S. Army Medical Corps officer, attests to the rapid and scalable benefits of TM in treating soldiers with combat trauma. Similarly, Dr. Vernon Barnes, with extensive experience teaching TM in military hospitals, emphasizes TM’s role as an adjunctive therapy that accelerates recovery from PTSD and traumatic brain injury, enabling patients to cement gains achieved through conventional evidence-based treatments.
Historically, TM has demonstrated resilience and mass appeal in post-trauma contexts, as illustrated by Dr. David Orme-Johnson’s work with survivors of the Armenian earthquake between 1989 and 1990. His group taught TM to thousands of people across societal strata, observing immediate emotional relief often accompanied by tears of release during initial practice sessions. Such accounts further validate the approach’s accessibility and acceptability in diverse, high-stress environments, reinforcing its potential for broad public health impact.
The authors of the meta-analysis highlight TM’s unique value proposition as a therapeutic method that minimizes the risk of retraumatization by avoiding the need for trauma re-exposure. This characteristic is critical, given that many conventional therapies can trigger distressing recall and compliance issues among PTSD patients. TM’s emphasis on autonomic nervous system regulation, fostered through its effortlessness and reproducibility, offers a gentler route to healing that may enhance patient adherence and long-term outcomes.
Despite these promising findings, the study’s authors advocate for large-scale, phase III clinical trials to firmly establish TM’s place alongside, or potentially in replacement of, existing PTSD treatments. Such trials would also clarify optimal dosing regimens, mechanistic pathways, and integration strategies within health care systems. Given TM’s favorable safety profile, scalability, and expansive evidence base, it stands poised to become a pivotal element in global mental health initiatives geared towards trauma recovery and stress reduction.
This meta-analysis, titled Systematic Review and Meta-Analysis of Transcendental Meditation for Post-Traumatic Stress Disorder, was co-authored by distinguished researchers David W. Orme-Johnson, Ph.D., Vernon A. Barnes, Ph.D., Brian Rees, M.D., and Jean Tobin. Their collaborative effort advances the science of meditation-based interventions and propels TM into the spotlight as one of the most effective, evidence-backed tools for PTSD symptom alleviation available today.
In conclusion, the convergence of rigorous meta-analytic data with biomolecular and neurophysiological evidence establishes TM as a transformative therapy with the potential to revolutionize PTSD treatment worldwide. By delivering rapid symptom relief through a non-invasive, non-trauma-focused pathway, TM presents a beacon of hope for millions suffering from the long shadows cast by trauma. As further large-scale studies emerge, the integration of TM into mainstream clinical practice may well mark a new era in the battle against the hidden wounds of psychological stress.
Subject of Research: People
Article Title: Systematic Review and Meta-Analysis of Transcendental Meditation for Post-Traumatic Stress Disorder
News Publication Date: 3-Apr-2025
Web References:
- https://www.mdpi.com/1648-9144/61/4/659
- https://www.mdpi.com/1648-9144/60/12/2050
- https://www.mdpi.com/2218-273X/15/3/317
References:
Orme-Johnson, D. W., Barnes, V. A., Rees, B., & Tobin, J. (2025). Systematic Review and Meta-Analysis of Transcendental Meditation for Post-Traumatic Stress Disorder. Medicina, 61(4), 659. DOI: 10.3390/medicina61040659
Image Credits: Maharishi International University
Keywords: Transcendental Meditation, PTSD, post-traumatic stress disorder, meta-analysis, trauma recovery, meditation, mental health, stress reduction, biomolecular mechanisms, cognitive function, cortisol, EEG, clinical psychology