The emergence and evolution of metabolic dysfunction-associated steatotic liver disease (MASLD) have garnered significant attention in the realm of medical research, particularly in the context of diverse populations. A recent article addresses the complex interplay between lifestyle factors, genetic predispositions, and metabolic disorders, contributing to a more nuanced understanding of MASLD in different demographic settings, especially within the Indian population. This response to the letter to the editor referring to the study on the profile of MASLD can provide critical insights into its implications on public health.
The researchers, Mohan and Jhaveri, open their discussion by contextualizing the increasing prevalence of metabolic disorders globally. They highlight that liver diseases, particularly those classified under MASLD, have become one of the leading causes of morbidity and mortality. The complexity of these diseases lies not only in their biochemical pathways but also in their socio-economic and cultural dimensions. As Western-style diets and sedentary lifestyles penetrate various societies, including India, the traditional protective barriers of metabolic health are eroded, leading to a surge in MASLD cases.
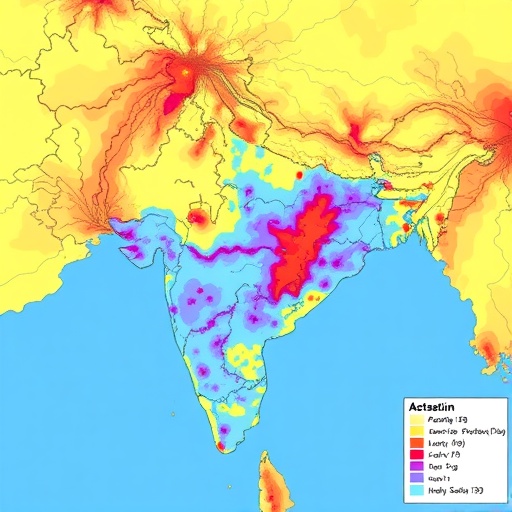
Central to the discourse is the MAP Study’s findings, which underscore the variability of MASLD prevalence across distinct Indian populations. The mapping of metabolic dysfunction and its associated liver disease emphasizes the necessity of tailored healthcare strategies. This geographic and demographic variability signifies that a one-size-fits-all approach in treatment and prevention is inefficient. Rather, an enriched understanding of local determinants influencing liver health is vital for effective intervention strategies that can address the specific needs of different groups within India.
Furthermore, Mohan and Jhaveri detail the multifactorial aspects of MASLD, including genetic susceptibility. The genetic diversity in populations contributes significantly to the risks associated with metabolic dysfunction. For instance, variations in genes related to lipid metabolism, alongside lifestyle choices, further complicate the clinical picture. Understanding these genetic factors assumes an essential role in developing personalized medicine approaches to monitor and treat individuals at risk of MASLD.
The authors also delve into the diagnosis and management of MASLD, asserting that early detection is crucial in preventing disease progression. They underscore the importance of liver function tests and imaging studies in recognizing steatosis early, which can facilitate timely interventions. However, the authors caution that access to these diagnostic tools remains unequal across various regions of India, thereby hampering efforts toward effective management of the condition.
In light of the rising cases, the researchers advocate for more robust public health initiatives aimed at educating communities about MASLD. Awareness campaigns that disseminate information regarding obesity, diabetes, and the implications of a high-fat diet are essential parts of a broader strategy to combat liver diseases. The emphasis must be on integrating lifestyle modification education into primary healthcare settings to empower individuals and communities to take charge of their health.
Mohan and Jhaveri also highlight the role of policy in shaping health outcomes related to MASLD in India. Existing frameworks must be revised to prioritize preventive strategies over reactive healthcare. Policymakers are urged to consider the unique population-specific characteristics when devising public health strategies that target the underlying causes of metabolic dysfunction. Investment in community health programs that promote physical activity and nutritional guidance can potentially alleviate the burden of MASLD on India’s healthcare system.
The letter responds to critiques and comments regarding the MAP Study, clarifying several key points about the methodology and findings. The authors address misunderstandings related to the statistical analyses employed in the study, insisting on the robustness of their conclusions. They further emphasize that their work serves as a foundation for future research, calling for more extensive studies to be conducted across the subcontinent to validate their findings.
Moreover, the authors argue that multidisciplinary collaborations are essential in addressing the rising tide of MASLD. Clinical researchers, epidemiologists, and public health officials must unite their expertise to conduct comprehensive studies that can generate actionable insights. By working in tandem, these professionals can not only report on prevalence rates but also devise interventions that are culturally relevant and economically feasible.
This discourse still hinges on the implications that the rising prevalence of MASLD can have on the Indian healthcare system as a whole. Healthcare providers must prepare to meet the growing demands for diagnosis and treatment, which will require substantial investment in both human and financial resources. The authors project that without proactive measures and significant investment in health infrastructure, India may face an overwhelming increase in liver-related health complications within this decade.
Ultimately, the response from Mohan and Jhaveri calls for a reinvigorated focus on understanding the nuances of MASLD within diverse populations. It is a call to action for researchers, clinicians, and policymakers alike to come together to combat this growing health crisis. The multi-faceted nature of MASLD underscores the necessity for inclusive and diverse strategies that cater to the varying needs and challenges faced by different populations.
As the dialogue around MASLD continues to evolve, collaborative efforts must persist, fostering a culture of knowledge sharing and research that bridges gaps in understanding. The implications of such research extend beyond academia; they reach into the lives of millions who are affected by metabolic disorders. With continued advocacy for better health policies and more precise public health initiatives, there is hope for a future where the burden of MASLD can be significantly reduced.
In conclusion, the correspondence by Mohan and Jhaveri not only clarifies the ongoing discourse surrounding MASLD but also highlights the urgent need for targeted interventions. As morbidity and mortality linked to metabolic dysfunction climb, it is imperative that health stakeholders unify their efforts to address this public health challenge substantively.
Subject of Research: Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD)
Article Title: Response to: Letter to the Editor Regarding ‘Profile of Metabolic Dysfunction-Associated Steatotic Liver Disease: Mapping Across Different Indian Populations (MAP Study)’
Article References:
Mohan, V., Jhaveri, K. Response to: Letter to the Editor Regarding ‘Profile of Metabolic Dysfunction-Associated Steatotic Liver Disease: Mapping Across Different Indian Populations (MAP Study)’.
Diabetes Ther (2025). https://doi.org/10.1007/s13300-025-01810-y
Image Credits: AI Generated
DOI: 10.1007/s13300-025-01810-y
Keywords: Metabolic Dysfunction, Steatotic Liver Disease, Public Health, India, Epidemiology, Personalized Medicine