In recent years, a growing body of research has illuminated the intricate relationship between physical health and mental well-being. A particularly striking interplay has been observed between keloids—a form of raised scar—and various psychiatric disorders. Keloids, which are the result of an overproduction of collagen during the healing process, can lead not only to physical discomfort but also significantly impact an individual’s mental health. A groundbreaking study recently published in Annals of General Psychiatry sheds light on this connection, providing genetic evidence that suggests a stronger link than previously understood.
The investigation into the association between keloids and mental disorders has revealed that individuals suffering from keloids often report elevated levels of psychological distress. This study presents compelling genetic evidence that may explain why these patients are more likely to experience mental health issues such as anxiety and depression. The researchers undertook a comprehensive analysis, examining both the genetic predispositions associated with keloids and the psychological profiles of affected individuals.
Within the confines of the study, the researchers explored the biological underpinnings of keloid formation. At its core, keloid development is driven by a dysregulated wound healing process. When skin is injured, the body naturally produces collagen to repair the damage. However, in individuals predisposed to keloids, this process goes awry, resulting in excessive collagen deposition and the formation of a keloid scar that extends beyond the original wound boundary. This physical manifestation of healing dysfunction can lead to significant psychosocial problems.
The research team employed advanced genetic sequencing techniques to uncover variants that may be implicated in both keloid formation and mental health disorders. By analyzing a cohort of individuals with keloids, they were able to identify specific genetic markers that are shared between these physical scars and mental health conditions. This genetic overlap suggests a possible shared pathophysiological mechanism, indicating that individuals with a genetic predisposition to keloids may also be at increased risk for developing mental health challenges.
Furthermore, the study highlights the role of systemic inflammation and stress in exacerbating both keloid formation and mental health issues. Chronic inflammation has been recognized as a contributing factor to various psychiatric disorders, and the persistent physical distress from keloids could serve as a source of psychological strain. The researchers posited that the physical discomfort and visibility of keloids could lead to social stigmatization, which may, in turn, contribute to feelings of depression and anxiety.
In addition to the genetic evidence, the study also outlined a variety of psychological assessments administered to participants. These assessments indicated that a majority of individuals with keloids reported heightened levels of anxiety, depression, and body image concerns. The impact of keloids on self-esteem was profound, with many participants expressing feelings of embarrassment or isolation due to their scars. This emotional toll further emphasizes the importance of considering psychological health in the treatment of patients with keloids.
The findings from this study carry significant implications for clinical practice. Healthcare providers treating patients with keloids should be aware of the potential psychological ramifications associated with this condition. A multidisciplinary approach that includes psychological support could enhance treatment outcomes for individuals dealing with both the physical and emotional challenges presented by keloids. Mental health screenings should be integrated into standard care protocols for keloid patients to identify those who may benefit from additional psychological support.
As the understanding of the mind-body connection continues to evolve, the insights gained from this study highlight the necessity for further research. Future studies should aim to explore the mechanisms underlying the genetic connections between keloid formation and mental health disorders. Additionally, longitudinal studies examining how the treatment of keloids impacts psychological well-being would provide further clarity on this complex relationship.
Patient education also plays a critical role in managing the psychological impact of keloids. Informing individuals about the potential for mental health issues associated with keloids can empower them to seek help proactively. Support groups and therapy focused on coping strategies may offer significant benefits, fostering resilience and providing communal support for those affected.
Moreover, the societal perception of keloids remains an important topic worthy of discussion. There is a pressing need for greater awareness and understanding within the medical community and the public at large regarding keloids and their implications. Reducing the stigma associated with visible scars could mitigate some of the psychological distress that accompanies keloid formation.
As this field of study progresses, it is clear that the relationship between keloids and mental health is complex, multifaceted, and worthy of continued exploration. This research marks a significant step toward unraveling these complexities, opening up avenues for future investigations into the genetic, biological, and psychological factors that intertwine health and mental wellness. The hope is that increased understanding will lead to improved patient outcomes, better support structures, and ultimately, a holistic approach to treating keloids and the associated mental health challenges they pose.
In conclusion, the association between keloids and mental disorders is a critical area of research that underscores the interconnectedness of physical and mental health. The genetic evidence presented in this study provides a foundation for further exploration into this link, demonstrating the necessity of addressing both the physical and psychological aspects of keloid treatment. As research continues to unfold, the implications for patient care, public perception, and future studies will undoubtedly shape a more compassionate and effective approach to managing the dual burdens of keloids and mental health disorders.
Subject of Research: Keloids and mental disorders
Article Title: Association between keloid and mental disorders: perspective from genetic evidence
Article References:
Zhan, Y., Tong, Y., Wu, X. et al. Association between keloid and mental disorders: perspective from genetic evidence.
Ann Gen Psychiatry 24, 42 (2025). https://doi.org/10.1186/s12991-025-00579-5
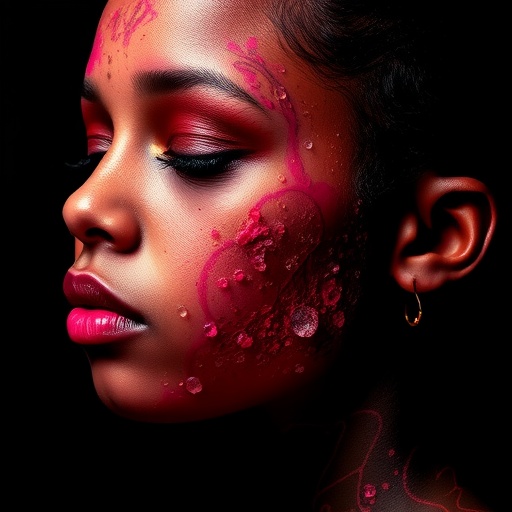
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12991-025-00579-5
Keywords: Keloids, mental health, genetics, anxiety, depression, collagen, inflammation, body image, healthcare, treatment outcomes.