In a groundbreaking exploration connecting mental health and metabolic dysfunction, recent research has unveiled a potential mechanistic link between insulin resistance and gut permeability in patients diagnosed with schizophrenia. Published in the 2025 issue of Schizophrenia, this study spearheaded by Couce-Sánchez and colleagues challenges traditional paradigms by delving deep into the biological intersections that may underlie both psychiatric and metabolic disturbances, thereby opening new horizons for therapeutic strategies.
Schizophrenia, a complex psychiatric disorder characterized by hallucinations, delusions, and cognitive impairments, has long been associated with an elevated prevalence of metabolic syndrome, including insulin resistance. Insulin resistance, a key pathophysiological factor in type 2 diabetes and cardiovascular diseases, involves diminished cellular responsiveness to insulin, which disrupts glucose homeostasis. However, the underlying reasons for this metabolic imbalance in schizophrenia patients have remained obscured, with antipsychotic medications often implicated as the primary culprits.
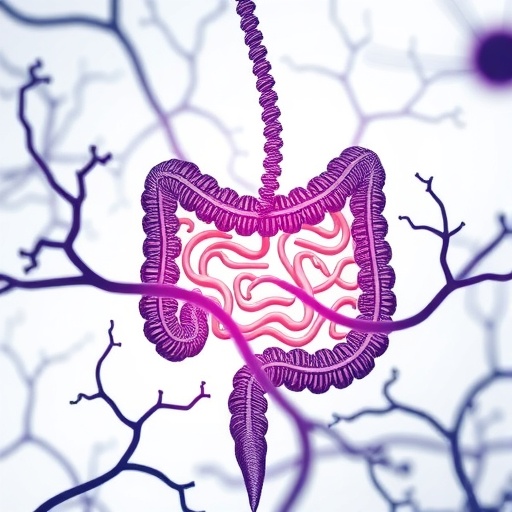
What this research brings to light is a novel focus on gut permeability—often referred to colloquially as a “leaky gut”—as a significant factor contributing to insulin resistance in schizophrenia. The gut barrier plays a crucial role in maintaining homeostasis by regulating the passage of nutrients while preventing harmful substances such as endotoxins and pathogens from entering systemic circulation. A compromised gut barrier can trigger systemic inflammation, which is increasingly recognized as a critical contributor to metabolic dysregulation.
The investigators employed a robust methodology that encompassed biochemical assays to measure markers of gut permeability alongside detailed assessments of insulin sensitivity among a cohort of patients with schizophrenia. Their data revealed a clear association between elevated gut permeability markers and insulin resistance indices, independent of antipsychotic treatment, suggesting that intestinal barrier dysfunction itself might drive metabolic alterations. This insight compels a reconsideration of how metabolic comorbidities manifest and persist in schizophrenia beyond medication side effects.
Further mechanistic insights stem from the interplay between gut microbiota, the immune system, and metabolic signaling. Dysbiosis—an imbalance in the microbial communities residing in the gut—has been documented in schizophrenia, and is known to impact the integrity of the gut lining. The resultant infiltration of lipopolysaccharides (LPS), a bacterial endotoxin, into systemic circulation may chronically activate inflammatory pathways, including cytokine cascades and oxidative stress, both implicated in the pathophysiology of insulin resistance. Thus, the gut-brain-metabolism axis emerges as a critical nexus in schizophrenia-related metabolic dysfunction.
These findings resonate with an expanding body of literature that recognizes schizophrenia not solely as a brain disorder, but as a systemic condition involving immune and metabolic dysregulation. The traditional siloed approach to treatment has inadequately addressed these peripheral comorbidities, often leading to suboptimal outcomes. Understanding gut permeability’s role signals a paradigm shift, advocating for integrated interventions targeting intestinal health alongside psychiatric care.
Clinically, this research proposes potential therapeutic targets that transcend conventional antipsychotics. Restoration of gut barrier integrity through dietary modulation, probiotics, prebiotics, or novel pharmacological agents could ameliorate insulin resistance and improve overall metabolic profiles in schizophrenia. Such strategies may also mitigate systemic inflammation, potentially impacting core neuropsychiatric symptoms, although this remains a fertile area for future exploration.
It is important to note the study’s sophisticated analytical design, which controlled for confounding variables such as age, medication type, duration of illness, and lifestyle factors including diet and physical activity. The rigorous control strengthens the argument that gut permeability alterations are intrinsic to the schizophrenia phenotype rather than an epiphenomenon of external influences.
Moreover, this investigation invites a re-examination of recent microbiome research, positioning gut permeability not merely as an outcome of microbial imbalances but as a driver of systemic metabolic and inflammatory states. The reciprocal interactions between microbiota and intestinal epithelial cells form a complex regulatory system, where perturbations can ripple through to influence distant organs, including the brain and pancreas.
The research also highlights the importance of longitudinal studies to track the evolution of gut permeability and insulin resistance over the course of schizophrenia, particularly in drug-naïve patients to delineate baseline biological changes from treatment effects. Such work could yield biomarkers predictive of metabolic risk, facilitating early intervention.
In addition to its medical implications, the study prompts broader philosophical reflections on the integration of mind and body medicine. The increasingly blurred boundaries between psychiatric and somatic disorders underscore the necessity of holistic approaches to health, grounded in systems biology and personalized medicine frameworks.
Future directions proposed by the authors include trials of gut-targeted therapies to assess their impact on insulin sensitivity and psychiatric symptoms alike. If successful, these interventions could revolutionize the management of schizophrenia, transforming a traditionally neurocentric model into a multidisciplinary endeavor that encompasses endocrinology, immunology, gastroenterology, and psychiatry.
Furthermore, this research may inspire investigations into other psychiatric disorders characterized by metabolic disturbances, such as bipolar disorder and major depressive disorder, to evaluate whether similar gut permeability-insulin resistance phenomena occur. Such comparative analyses could uncover universal or disorder-specific pathophysiological mechanisms.
Importantly, the study’s findings challenge stigma surrounding schizophrenia by elucidating biological underpinnings for its associated health complications. Recognizing these systemic pathologies legitimizes comprehensive medical care for affected individuals, fostering improved quality of life and reduced mortality.
In conclusion, the pioneering work by Couce-Sánchez et al. lays a critical foundation for understanding the intertwined relationship between gut health and metabolic impairment in schizophrenia. By illuminating gut permeability as a pivotal factor in insulin resistance, this study not only advances scientific knowledge but also charts a course toward innovative, integrated treatment paradigms that may transform patient outcomes in this challenging disorder.
Subject of Research: Insulin resistance and gut permeability in schizophrenia patients
Article Title: Insulin resistance in patients with schizophrenia: is it related to gut permeability?
Article References:
Couce-Sánchez, M., Dal Santo, F., González-Blanco, L. et al. Insulin resistance in patients with schizophrenia: is it related to gut permeability? Schizophr 11, 145 (2025). https://doi.org/10.1038/s41537-025-00688-w
Image Credits: AI Generated