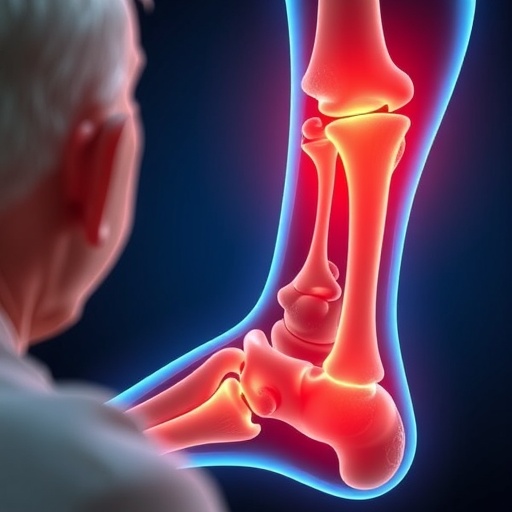
Aging has long been recognized as a critical factor that impairs the body’s ability to repair bone fractures, contributing to prolonged recovery times and increased complications in older adults. Despite extensive research into local bone biology, the systemic molecular mechanisms underlying this decline have remained poorly understood. Now, a groundbreaking study from Duke University uncovers a pivotal role for apolipoprotein E (ApoE), a liver-derived circulating protein, in inhibiting bone regeneration during aging. This discovery not only elucidates an age-associated molecular brake on bone repair but also offers a novel therapeutic avenue to rejuvenate skeletal healing in the elderly.
Bone repair is an intricately choreographed process involving the activation and differentiation of skeletal stem and progenitor cells into osteoblasts, the specialized cells responsible for new bone formation and mineralization. In youthful individuals, this cascade unfolds swiftly and efficiently to restore bone integrity post-injury. However, this reparative capability diminishes substantially with age, leading to slower healing and a greater risk of fracture nonunion or poor-quality bone formation. The Duke research team sought to dissect the systemic factors contributing to this age-dependent decline using murine fracture models matched for young versus old cohorts.
Through comprehensive molecular and histological analyses, the scientists identified significantly elevated circulating levels of ApoE in aged mice, suggesting a hepatic contribution to systemic aging signals. ApoE is traditionally characterized for its role in lipid metabolism and cardiovascular disease, but here, it emerges as a potent inhibitor of skeletal regeneration. The team demonstrated that ApoE interferes directly with the Wnt/β-catenin signaling pathway, an essential intracellular cascade that governs progenitor cell differentiation into osteoblasts. Suppression of β-catenin activity effectively stalls bone formation at an early stage by preventing maturation of the bone-forming cell lineage.
Mechanistically, elevated ApoE exerts its inhibitory effects by binding to the Lrp4 receptor expressed on bone marrow stromal cells. This receptor-ligand interaction disrupts downstream β-catenin signaling, thereby imposing a molecular “brake” on the osteogenic machinery. Importantly, the researchers employed neutralizing antibodies to block ApoE activity in aged mice, which led to a remarkable restoration of β-catenin signaling and resumption of osteoblast differentiation. This intervention translated into significantly improved fracture healing, characterized by more robust callus formation and bone bridging at injury sites, approximating the quality and speed of repair observed in young animals.
Lead investigator Dr. Gurpreet Singh Baht emphasized the paradigm-shifting nature of the findings: “Aging doesn’t merely slow down bone repair; it actively suppresses it via systemic signals stemming from distant organs like the liver. By neutralizing ApoE, we effectively release this molecular brake and enable aged bones to repair themselves with youthful efficiency.” This revelation underscores the potential of targeting circulating systemic factors, rather than solely focusing on local bone environment manipulation, to develop innovative therapeutics for aging-associated skeletal fragility.
The reversal of age-imposed inhibition of bone healing observed in these experiments was particularly striking. Even in advanced age, progenitor cells retained their intrinsic regenerative potential but were held in check by ApoE-mediated signaling. When this blockade was removed, the bone-forming program reignited robustly, highlighting the dynamic plasticity of the aged skeletal system and opening new therapeutic windows to enhance musculoskeletal health in the elderly population.
Beyond advancing fundamental understanding of bone biology, this research carries significant clinical implications. Fractures in older adults consistently lead to prolonged hospitalization, increased morbidity, and sustained loss of independence. Current treatments emphasize mechanical stabilization of fractures but offer limited options to biologically accelerate or improve healing outcomes. The identification of ApoE as a systemic and modifiable inhibitor of bone regeneration provides a promising target to augment repair processes, reduce fracture healing times, and minimize long-term disability.
Notably, this work also shifts the scientific perspective toward appreciating the liver’s unanticipated role as a regulator of skeletal regeneration. Traditionally, bone fracture repair research has concentrated on local cues at injury sites, such as growth factors and cellular cross-talk within the bone marrow niche. The discovery that hepatic-secreted ApoE circulates systemically to influence distant bone cell behavior highlights the complex organ-to-organ communication pathways that modulate tissue repair during aging.
Experimental methodologies employed by the Duke team encompassed robust animal fracture models, molecular diagnostics including gene expression and protein interaction assays, as well as comprehensive histological evaluations. These multi-modal approaches strengthened the mechanistic conclusions and confirmed that targeting ApoE with neutralizing antibodies could serve as an effective therapeutic intervention. The data illuminate a previously uncharted axis connecting liver metabolism, aging physiology, and bone regeneration biology.
This study’s findings open exciting new frontiers for regenerative medicine strategies aimed at reactivating intrinsic repair mechanisms through systemic modulation rather than localized treatments alone. Targeting ApoE and its pathway could provide a safer, systemic approach to enhance fracture healing without the risks associated with direct cellular manipulation or high-dose growth factor therapies. Such systemic therapy has the potential to broadly benefit aging populations by reinstating the natural programs of skeletal renewal critical for mobility and quality of life.
As the global population ages, with a concurrent surge in age-related bone diseases and fractures, interventions that restore robust and timely bone regeneration become paramount. This research not only identifies a novel molecular culprit—ApoE—as a driver of bone repair failure in aging but also defines a clear, actionable therapeutic target. The prospect of neutralizing age-associated circulatory inhibitors to safely reinvigorate fracture healing represents a transformative advance in geriatric orthopedics.
In conclusion, the work led by Dr. Baht and colleagues marks a major leap forward in understanding how systemic aging factors suppress bone regeneration. By unveiling ApoE as a critical hepatic-derived inhibitor that dampens progenitor cell differentiation via Lrp4–β-catenin signaling disruption, the study lays a molecular foundation for innovative therapies designed to restore youthful healing capacity in aged bone. These insights herald a new era in fracture care where modulation of systemic aging signals complements local orthopedic interventions, ultimately improving outcomes and preserving function for millions of older adults worldwide.
Subject of Research: Animals
Article Title: Neutralizing hepatic apolipoprotein E enhances aged bone fracture healing
News Publication Date: 22-Jan-2026
References: DOI: 10.1038/s41413-025-00489-y
Image Credits: Dr. Mingjian Huang, Ms. Kristin Molitoris, Dr. Gurpreet Singh Baht from Duke University, USA
Keywords: Bone diseases, Muscle diseases, Aging populations, Orthopedics, Molecular biology, Cell biology, Regenerative medicine, Physiology, Animal models, Geriatrics, Medical treatments