Cataracts stand as one of the most pervasive causes of blindness globally, disproportionately impacting populations in low- and middle-income countries where access to advanced medical technologies remains limited. Traditionally, the most effective treatment for cataracts has been phacoemulsification, a surgical procedure utilizing ultrasound waves or laser energy to break apart and remove the clouded natural lens of the eye. Though this approach has seen significant advancements, the reliance on expensive, high-tech laser systems has created a barrier to availability in resource-constrained settings. Many patients in these regions face longer recoveries and suboptimal outcomes simply because the necessary sophisticated equipment is beyond their reach.
In an effort to bridge this critical gap in global eye care, a progressive research team from the University of South Florida has conceived an innovative, low-cost laser system poised to revolutionize the approach to cataract surgery in underserved areas. Drawing upon the principles of optical engineering and photonics, their method employs a millisecond-pulsed diode laser, constructed from commercially accessible components, to perform the phacoemulsification process. This marks a radical departure from the traditionally used femtosecond lasers, which, despite their precision, are prohibitively expensive and complex for widespread deployment in lower-income healthcare environments.
To validate the efficacy and safety of their novel apparatus, the researchers engaged in rigorous computational simulations alongside empirical laboratory experiments utilizing tissue-mimicking phantoms. These studies demonstrated that the diode laser delivers sufficient energy to effectively liquefy the cataract-like material without inflicting collateral thermal or mechanical damage to the adjacent healthy ocular structures. The laser operates within a narrowly confined spatial domain, ensuring the controlled application of heat strictly at the interface of the targeted cataract, thereby minimizing risks typically associated with conventional techniques.
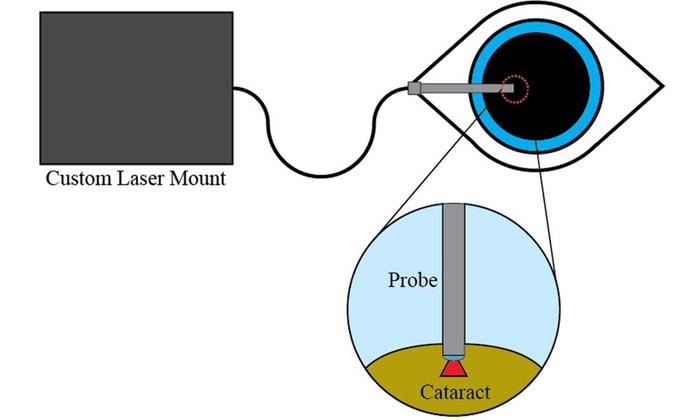
The underpinning technology centers around the delivery of near-infrared light pulses via a bespoke surgical probe, meticulously designed to integrate seamlessly with existing ophthalmic surgical workflows. The pulse duration and energy parameters have been optimized to balance maximal cataract disruption with minimal thermal diffusion, a critical factor in preserving surrounding tissue integrity. By employing this carefully calibrated pulsed delivery system, the research team hopes to offer a viable alternative that maintains safety and effectiveness while drastically reducing both cost and equipment complexity.
Mitchell Harrah, the PhD candidate who spearheaded this investigation, emphasizes that this approach could transform cataract surgery accessibility across rural and economically disadvantaged regions. The affordability and compact size of the diode laser system reduce infrastructural demands and the need for extensive operator training often associated with traditional laser platforms. Such democratization of surgical technology has the potential to alleviate the growing global cataract burden exacerbated by aging populations, particularly in parts of the world where eye care resources are scarce.
Importantly, the precision control of the laser’s thermal effects represents a technological advancement that not only protects ocular anatomy but also shortens patient healing times. Conventional ultrasound-based phacoemulsification invariably raises concerns about collateral tissue trauma, contributing to postoperative inflammation and delayed recovery. By contrast, the diode laser’s targeted energy application mitigates these risks, potentially speeding visual rehabilitation and improving overall surgical outcomes.
The system’s design also considers integration with existing ophthalmic infrastructure. The custom surgical probe is engineered for ergonomic handling and is compatible with standard operating microscopes, enabling surgeons to adapt quickly to its use. Furthermore, the reliance on diode lasers—a technology widely utilized in telecommunications and other industries—ensures that replacement parts and maintenance can be sustained with relative ease and cost-effectiveness.
Computational modeling underpinning this research provides a robust framework for further refinement and customization of laser parameters tailored to patient-specific cataract densities and morphologies. Such predictive capabilities could culminate in personalized surgical protocols that optimize energy dosage, reducing variability and enhancing reproducibility of results across diverse clinical scenarios. This capability heralds a future where precision medicine principles are applied even in resource-constrained surgical environments.
While these preliminary findings are compelling, the authors of the study acknowledge that clinical validation is the critical next step. Trials involving human subjects will be essential to assess the laser system’s real-world safety profile, efficacy, and long-term outcomes. If successful, this technology could disrupt existing paradigms of cataract surgery, shifting from a model dependent on centralized, high-cost equipment to one characterized by portability and affordability without compromising precision.
The implications of widespread adoption of this low-cost laser phacoemulsification system extend beyond cataract treatment alone. It serves as a case study in the potential for engineering innovation to address significant health disparities by tailoring advanced technologies to the constraints and needs of underserved populations. This work exemplifies how cross-disciplinary collaboration between photonics researchers, biomedical engineers, and clinicians can birth solutions with profound public health impact.
Ultimately, the research conducted by Harrah and colleagues signals a hopeful horizon for millions deprived of sight-restoring surgery due to economic and infrastructural limitations. By pioneering an accessible laser-based alternative to traditional cataract extraction methods, this breakthrough not only promises to lessen the global blindness burden but also showcases the transformative role of scalable technology in democratizing healthcare.
With an aging world population and cataract prevalence projected to rise steadily, innovations of this sort are urgently needed. The research community and global health policymakers alike will be watching closely as this low-cost optical system advances through the pipeline toward clinical implementation. Should it meet expectations, millions who once faced blindness may soon regain their vision, fundamentally altering quality of life on a massive scale.
Subject of Research: Low-cost laser system for cataract phacoemulsification
Article Title: Low-cost optical system for laser phacoemulsification of cataracts
News Publication Date: 29-Apr-2025
References:
Harrah M., et al., “Low-cost optical system for laser phacoemulsification of cataracts,” Biophotonics Discovery, 2(2), 022304, doi:10.1117/1.BIOS.2.2.022304
Image Credits: Mitchell Harrah
Keywords
Health and medicine, Applied optics, Laser systems, Semiconductor lasers, Vision disorders, Cataracts